
“Bringing Patient Safety To Life”
What’s worked, what hasn’t, and what to do about it.
October 17th & 18th, 2023
The conference sessions are recorded and available!
CE credits are no longer available for 2023.
HOW TO VIEW THE RECORDED PRESENTATIONS
The conference presentations are posted on the conference event portal. If you registered for the live conference, all presentations, and supporting materials, are available for you to view. To view the recorded presentations, log into the event portal just as you did for the live event using the link found in your registration confirmation and enter your attendee confirmation code (you can find your attendee confirmation code at the very bottom of your registration confirmation email, if you can’t obtain it, please contact Amelina Kassa at akassa@qualityhealth.org.) Once you are logged into the portal, click on the “Info” tab at the top of the page (most left tab). The presentations, slides, and supporting materials will all be posted below on the page sorted by presentation date and time.
HOW TO REGISTER FOR THE CONFERENCE TO WATCH THE RECORDED PRESENTATIONS
Didn’t get to attend the live event? No worries, we’ve got you covered! To register, please contact Amelina Kassa at akassa@qualityhealth.org. Amelina will get you registered. Conference fees and discounts apply. See the registration tab for more information.
C.E. Credit Information:
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2023 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. Upon receipt of your survey/CE application, we will either send you a certificate(s) or for Nursing Contact Hours we will send you a required questionnaire about each presentation.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
CE CREDITS FOR ALL PRESENTATIONS ARE NO LONGER AVAILABLE
In the event portal, toward the top of the “General Info” page is a section called “How to get educational credits.” In this section is a link to a CE application form used for the recordings. Use this for all recorded presentations. Upon receipt of your CE application, we will send you the certificate(s).
ABOUT THE CONFERENCE
Welcome to our 20th conference! The theme is “Bringing Patient Safety To Life: What’s worked, what hasn’t, and what to do about it.” The conference is focused on solutions to problems rather than the problems themselves. We could talk about how to chase adverse events better, instead we’ll discuss the National Action Plan to Advance Patient Safety. We could lament about healthcare mergers & acquisitions, but we’d prefer to present ways to sustain safety programs when leadership changes (no, it doesn’t involve your CV). We could ignore climate change, but you’ll hear about a tool designed to help health professionals connect with patients and colleagues to respond to the health risks of climate change (no, it doesn’t involve wearing a mask).
Keynote Presentations
Umair A. Shah, MD, Secretary of Health, Washington State: Opening Keynote
Secretary Shah will deliver the opening keynote. Appointed by Governor Jay Inslee in December 2020. He was responsible for the state’s COVID-19 response and vaccination efforts. He is the first Asian-American physician of South Asian descent to serve in this leadership role in the history of Washington. He is a strong advocate for patients and equity stemming from his experience as an emergency department physician at the Michael E. DeBakey Veterans Affairs Medical Center in Houston for well over twenty years.
Karthik Sivashanker, MD: “Operationalizing Racial Justice and Equity in Health Care”. Dr. Sivashanker is the Vice President of Equitable Health Systems in the Center for Health Equity at the American Medical Association. He will discuss a new framework for advancing racial justice and equity in the health care arena by leveraging high-performance quality and safety practices to systematically make inequities visible and to address and resolve them as an integral part of health care practice.
Tejal Gandhi, MD: “Emerging from COVID: Re-Energizing our Approach to Achieving Zero Harm”. This won’t be a Covid commiseration conference, although I do miss the lack of car traffic. You probably know Dr. Gandi as the former President and CEO of the National Patient Safety Foundation (NPSF) or Chief Clinical and Safety Officer at the Institute for Healthcare Improvement (IHI). Now, as Chief Safety and Transformation Officer at Press Ganey, she is responsible for advancing the Zero Harm movement and developing innovative health care transformation strategies. Dr. Gandi will present the “bright spots”, innovations and lessons learned while we were up to our elbows in alligators.
Patricia McGaffigan: “Strengthening our Resilience – Implementation of Safer Together: A National Action Plan to Advance Patient Safety”. Patricia is President, Certification Board for Professionals in Patient Safety, and Vice President at IHI where she is IHI’s senior sponsor for the National Steering Committee for Patient Safety. Patricia will present on the National Action Plan to Advance Patient Safety. Despite substantial effort over the past 20 years, preventable harm in health care remains a major concern in the United States. The Plan includes 17 recommendations to advance patient safety and offers actionable solutions for a clear path forward to recover from setbacks that occurred during the pandemic and to advance and sustain the positive gains based on lessons learned over two decades of systems safety improvement work.
Saul Weingart, MD: “Finding the Patient in Patient Safety”
Dr. Weingart is Professor of Medicine at Brown University’s Warren Alpert School of Medicine. He served as President of Rhode Island Hospital and Hasbro Children’s Hospital, CMO and SVP of Medical Affairs at Tufts Medical Center and VP for Quality Improvement and Patient Safety at Dana-Farber Cancer Institute. Enthusiasm for patient and family engagement makes a number of assumptions about the opportunities and limitations of patient and family engagement that warrant closer review This session will draw on 20 years of empirical research, industry best practice, and participants’ experience to better understand the current state of knowledge and practice and to identify promising strategies to engage patients and families in making healthcare safer.
In addition to the keynotes there are nine incredible breakout sessions with regional, national and international experts, thought leaders and your colleagues. Here are some of the topics. You’re encouraged to visit the presentation tab for more details.
- Structuring patient safety programs to survive leadership changes and other challenges.
- Impact of climate change on patient safety and quality.
- Transformative change: advancing cultural safety and relationship-based approaches to healing.
- Using artificial intelligence to improve the patient-provider experience.
- Staffing and safety: using computer modeling to reveal the drivers of nurse workload and missed care.
- Creation of a National Patient Safety Board (NPSB).
- Improving patient and provider communication.
About the Northwest Patient Safety Conference
Now in its 20th year, the Northwest Patient Safety Conference is the only event of its kind in the Western US, uniting healthcare professionals, providers, patients, families, and caregivers from all care settings for networking and engaging in sessions with industry thought leaders invested in improving the patient experience. This year’s conference is our second virtual conference, and our second year in collaboration between the Washington Patient Safety Coalition, the Oregon Patient Safety Commission, and the Health Quality BC.
Members of the conference committee who are putting on this fantastic conference
Jonathan Stewart – Chair Jamie Leviton
Amelina Kassa Jeff Goldenberg
Andrea Wnuk Karen Brigham
Anita Sulaiman Naomi Kirtner
David Birnbaum Rex Johnson
Farinaz Havaei Rhonda Bowen
Jackie Valentine Valerie Harmon
About the Washington Patient Safety Coalition
The Washington Patient Safety Coalition brings together a diverse group of participants to focus on achieving common patient safety goals. Our mission is to improve safety for patients receiving health care in Washington, in all care settings, with a vision of safe care for every patient, every time, everywhere. The WPSC is a program of the Foundation for Health Care Quality, a nonprofit organization dedicated to providing a trusted, independent, third-party resource to all participants in the health care community – including patients, providers, payers, employers, government agencies, and public health professionals.

This year’s conference is presented in collaboration with the Oregon Patient Safety Commission and Health Quality BC.
Total presentations: 14
HOW TO REGISTER FOR THE CONFERENCE TO WATCH THE RECORDED PRESENTATIOINS
To register, please contact Amelina Kassa at akassa@qualityhealth.org. Conference fees and discounts apply.
Fees:
- Healthcare professionals and anyone seeking continuing educational credits, $75
- Patients, their families, and students, Free
- Discounts are offered for registrants with CPPS, CPHQ and BCPA certifications.
Payments accepted: all major credit cards via PayPal.
Continuing educational credits: Attendees are eligible for Nursing contact hours, CPHQ, CPPS and BCPA educational credits. These may be acquired by attending the live sessions or watching the recorded sessions up to the next conference in October, 2024.
*Recorded educational credit availability is determined by the accrediting organization. Attendees will request CE credits via a conference survey following the conference or via a form on the recorded conference website. PLEASE NOTE THE CREDIT AMOUNTS MAY CHANGE IF THE AGENDA CHANGES.
| Credit Type | Total Credits for Conference | Credits Available for Recordings |
| BCPA | 4 JEDI 10 general Click here for Approved Program Content (live & recorded) |
Yes – up to the 4 JEDI and the 10 general |
| Nursing Contact Hours |
14.8 total available 8.8 for attending live Approved by the California Board of Registered Nursing, Provider Number CEP 16359 for 14.8 contact hours |
Yes, up to the 14.8 total |
| CPHQ | 14 total 8 for attending live |
Yes, up to the 14 total |
| CPPS | 14 total 8 for attending live |
Yes, up to the 14 total |
Registration questions? Contact wpsc@qualityhealth.org or call Steve Levy, Executive Director, 206-204-7383.
Opening Keynote - Umair A. Shah, MD, MPH, Secretary of Health, Washington State
As we phase out of COVID-19 as our main programming and communications focus, many state, territorial, and local public health departments find themselves asking, where do we go from here? This presentation will offer some of the key strategies the Washington State Department of Health deployed during the COVID pandemic, and how we are building on these successes to inform current and future public health opportunities. From our focus on equity, innovation, and engagement in our transformational communications plan, to our tech-driven approach to emergency preparedness, we will offer participants insight into how Washington went from ground zero of COVID-19 in the U.S. to a state with one of the highest vaccination and lowest mortality rates.
Learning Objectives:
1. Discuss at least one challenge and one success of the WA DOH during the COVID-19 emergency.
2. Identify at least one successful method and one communication strategy learned from the pandemic to increase public awareness.
3. Compare techniques utilized by the department to increase awareness of preventive measures.
Karthik Sivashanker, MD - Operationalizing Racial Justice and Equity in Health Care
This interactive session will cover 1) foundational concepts on health equity, including the various types of bias and discrimination commonly seen in healthcare; and. 2) a new framework for advancing racial justice and equity in the health care arena by leveraging high-performance quality and safety practices to systematically make inequities visible and to address and resolve them as an integral part of health care practice.
Learning Objectives:
1. Define core concepts related to equity and healthcare
2. Describe five key drivers for eliminating inequities by focusing on quality and safety
3. Identify specific strategies for effectively leveraging existing quality/safety infrastructure and processes to advance equity
David Birnbaum, Ph.D. and Dr. Naz Havaei - Learning from Things that Worked & Things that Didn’t: How Future Patient-Care Quality and Safety Programs Should be Structured to Survive Challenges and Leadership Change.
This session will focus on how patient-care quality and safety programs should be structured to create cultures that can survive challenges and leadership change, and ensure they continuously lead to actual improvements. You will learn how to avoid repeating an inherent failure cycle often caused by differences in opinion and turnover at critical leadership positions, rather than programmatic shortcomings.
Learning Objectives:
1. Become aware of important historical program innovations that became lost to institutional memory
2. Recognize reasons from the research literature that explain why programs with successful impact like these may fail to persist
3. Learn the location of practical instructions archived from these past programs to inform bold future policy & practice alternatives.
Mark Matthew and Meghann Brinoni - Transformative Change in British Columbia: Advancing Cultural Safety and Relationship Based Approaches to Healing
Widespread and systemic racism, stereotyping, and discrimination against Indigenous peoples in the British Columbia (BC) health systems have resulted in a range of negative impacts, up to and including, harm and even death. This session will review advancements made in BC to affect systems change and improve Indigenous patient safety. The creation of BC Cultural Safety and Humility organizational standard – the first of its kind in Canada, and emerging work in applying restorative approaches to prevent and heal from health care harms will be discussed and explored.
Learning Objectives:
1. Understand the need for a systems change approach to improving safety for Indigenous people in health care
2. Identify evolving approaches to how organizations can address systemic racism in their institutions
3. Describe the principles of restorative approaches and how they might be applied to complaint management and dispute resolution
Stefan Wheat, MD - Navigating the Nexus: Examining the Interplay Between Patient Safety, Quality, and Climate Change in Healthcare
In this interactive session, we will explore the profound impact of climate change on patient safety and quality in healthcare. Climate change is no longer a distant threat but an immediate concern that demands the attention of those dedicated to ensuring safe and high-quality care.
We will delve into the relevance of climate change to healthcare professionals, highlighting the interconnectedness of environmental factors and patient well-being. Just as the pandemic exposed unforeseen challenges such as distancing procedures, material shortages, and provider mental health, we will uncover climate change equivalents that may disrupt safety and quality in healthcare delivery.
Furthermore, we will explore how climate change alters the very fabric of healthcare delivery, extending the responsibilities of safety and quality beyond traditional definitions and the confines of hospital walls. We will showcase ClimateRx, a promising initiative that explores solutions to climate-related healthcare challenges.
Lastly, we will examine the health threats posed by climate change, including access to care and shortages, with a focus on the patient care experience.
Join us for this enlightening session as we explore the intricate relationship between climate change, patient safety, quality, and the future of healthcare.
Together, we can build a sustainable and resilient healthcare system capable of weathering the storm of climate change.
Learning Objectives:
1. Understand the profound impact of climate change on patient safety and quality in healthcare, recognizing the urgent need for healthcare professionals to address this immediate concern.
2. Explore how climate change transforms the landscape of healthcare delivery, expanding the responsibilities of safety and quality beyond traditional definitions and hospital boundaries, and recognizing the importance of proactively addressing climate-related healthcare challenges.
3. Examine the health threats posed by climate change, including access to care and shortages, and gain insights into the patient care experience in the context of climate change, emphasizing the need for equitable and resilient healthcare systems.
Tejal Gandhi, MD - Emerging from COVID: Re-Energizing our Approach to Achieving Zero Harm
This presentation explores the broader definition of harm beyond physical safety, and the importance of addressing inequities to achieve zero harm. In this session, Dr. Gandhi shares strategies and tactics to show how leading organizations are innovating and transforming a culture and leveraging high reliability to build engaged, resilient care teams that deliver safe, high-quality care and the optimal patient experience.”
Learning Objectives:
1) describe a broader definition of harm, including harm to patients and the workforce across the continuum
2) describe the impact of covid on all types of harm and inequities causing harm
3) understand strategies to advance the goal of zero harm using high reliability approaches
Saul Weingart, MD - Finding the Patient in Patient Safety
Patient and family engagement has been heralded as an untapped resource for promoting patient safety in clinical settings and in the community. Enthusiasm for this concept makes a number of assumptions about the opportunities and limitations of patient and family engagement that warrant closer review. What do we know about the ability of patients and families to recognize medical errors and adverse events? What do we know about their ability to escalate their concerns to a responsible clinician? How confident are we about patients’ and families’ willingness and ability to embrace safety-oriented behaviors, especially in the setting of an acute or serious illness? This session will draw on 20 years of empirical research, industry best practice, and participants’ experience to better understand the current state of knowledge and practice and to identify promising strategies to engage patients and families in making healthcare safer.
Learning Objectives:
1. Assess what we know about patients’ experience of medical error.
2. Analyze research about patients’ ability to identify errors.
3. Identify opportunities to engage patients and families in improving patient safety
Panel Discussion - "I Had to Say Something: Role models for cultures of psychological safety" The Washington Patient Safety Speak-Up Award Winners discuss their experience of speaking up for safety.
The Washington Patient Safety Coalition (WPSC) Speak-Up! Award is a statewide recognition program to celebrate individuals and teams at Washington healthcare organizations who voice their concerns to keep patients and staff safe. Their actions, and their organizations, serve as a models of positive cultures of safety.
Three Speak-Up winners share the aspects of their organizations’ safety cultures that facilitated their ability to prevent patient harm. They will share lesson’s learned, and the improvements and results due to speaking up.
Learning objectives
1. Describe characteristics of successful cultures of psychological safety
2. Identify how psychological safety contributes to better patient outcomes, lower staff burnout, and how organizations sustain psychological safety.
3. List strategies to overcome barriers to reporting adverse events and ways to increase reporting.
Harjinder Sandhu - Artificial Intelligence: improving the patient-provider experience in healthcare
AI is transforming the world, this session will preset applications and examples of artificial intelligence that are transformational to patients and providers including how AI is improving the patient journey from enhancing patients and provider collaboration, improving the diagnostic process to alleviating provider fatigue and burnout.
Learning objectives:
1. Participants will understand how specific applications of AI can support patient care and the implications of their application to outcomes.
2. Participants will learn how AI enhances patient-provider engagement throughout the patient journey.
3. Participants will understand the implications of incorporating AI as a tool for patients and providers.
Sara Kim, Ph.D. - Tuning in to Prevent Harm: The Art of Impeccable Listening
In this session, participants will learn about barriers to and facilitators of listening. Some of the questions posed in the session will be: What is active listening? How would I know I am an impeccable listener? How do I overcome key barriers to becoming a more attentive listener? Participants will have opportunities to practice and share with others the mindset and skills that have shaped their listening practices.
Learning Objectives:
1. Know my barriers to making active listening a challenge
2. Set intentions to shape my mindset and words
3. Demonstrate deep listening in face of high emotions
Panel Discussion: The landmark Federal legislation that would establish a National Patient Safety Board (NPSB)
Learn about the landmark Federal legislation that would establish a National Patient Safety Board (NPSB), modeled in part after successful entities in the transportation industry. This session will describe a proposed federal independent agency, the National Patient Safety Board (NPSB) modeled in-part after the National Transportation Safety Board (NTSB). It would support agencies in monitoring and anticipating adverse events with artificial intelligence, conduct studies, create recommendations and solutions to prevent medical error, and leverage existing systems and bring key learnings into practice.
Learning Objectives:
1. Learn about the landmark Federal legislation that would establish a National Patient Safety Board (NPSB), modeled in part after successful entities in the transportation industry.
2. Understand the NPSB approach to preventing and reducing patient safety events in healthcare settings.
3. Learn how the NPSB would complement existing agencies in monitoring and anticipating patient safety events with artificial intelligence, provide expertise to study the causes of errors, create recommendations and solutions to prevent future harms, and leverage existing systems to bring key learnings into practice.
Panelists include:
Dr. Karen Feinstein, President and Chief Executive Officer of the Jewish Healthcare Foundation (JHF) and its three operating arms, the Pittsburgh Regional Health Initiative (PRHI), Health Careers Futures (HCF), and the Women’s Health Activist Movement Global (WHAMglobal).
Marty Hatlie, J.D, CEO, Project Patient Care (PPC), co-developer of the H2Pi – Healthcare & Patient Partnership Institute, and President of Partnership for Patient Safety (p4ps).
Lisa McGiffert, President, PSAN (Patient Safety Action Network)
Helen Haskel, MA is founder of the nonprofit patient safety organization Mothers Against Medical Error and president of Consumers Advancing Patient Safety.
Patrick Neumann - New computer models reveal the drivers of nurse workload, missed care, and other quality threats in healthcare systems.
This interactive talk will present some of the latest research in using computer simulation of healthcare systems to understand how the design of the healthcare system affects nurse workload and, consequently, healthcare quality indicators such as “missed care”. We will present a brief non-technical overview of the modelling approach and share results from our most recent models in a hospital med-surg unit. Future applications and directions for these kinds of ‘digital twin’ models will be discussed.
Learning Objectives:
1. Introduction to the basic idea of computer simulations in healthcare
2. Increased Awareness of how nurse workload drives care quality
3. An understanding of the factors driving nurse workload and how simulation can reveal their level of impact
Anna Kristina Moroz, PhD - The promotion of trauma-informed care practice in medical settings
One of the primary goals of trauma-informed care practice is to actively work to prevent re-traumatization of individuals accessing services such as healthcare (SAMHSA’s Trauma and Justice Strategic Initiative 2014). This goal is based on the fact that many patients engaging with the medical system have experienced trauma in their lives that healthcare providers may or may not be privy to. Given the perceived power dynamic in providers’ offices, providers, nurses, and other patient facing employees such as phlebotomists should be especially cognizant of how their actions may result in the (re)traumatization of patients and should actively work to mitigate potential harm in order to improve medical system-patient relationships. In addition to providers, all individuals working in healthcare settings (e.g., front desk agents, medical directors of patient safety, and upper management) should be aware of trauma-informed care as there is a great potential for the (re)traumatization of patients when patients interact with bureaucracies (SAMHSA’s Trauma and Justice Strategic Initiative 2014). This session will describe the pervasiveness of traumatic experiences in our society and the deleterious effects this has on a person’s health. The session will subsequently describe the components of trauma informed care practice as described by Hess (2019): (1) establish safety, (2) be collaborative, (3) be trustworthy and transparent, (4) provide choice, and (5) empower. Examples from the academic literature, my personal medical trauma, and online materials (e.g., blog posts) will demonstrate why healthcare workers and administrators should adhere to these principles. I will argue that there are many small actions that healthcare workers and administrators can take to improve experiences for patients through a trauma-informed lens which can result in greater feelings of safety by patients while accessing medical care thereby leading to better relationships with patients and better health outcomes. I believe that admirable medical professionals and trustworthy institutions resolve to improve their practices with the goal of improving patient experiences and health outcomes in line with patient goals, and I believe that medical professionals and institutions implementing trauma-informed care in our society have the power to help with systemic issues present in the healthcare system. Works Cited: Hess, S. (2019, May 15). Five How-Tos of Trauma-Informed Practice. Health & Medicine Policy Research Group. https://hmprg.org/wp-content/uploads/2019/05/How-Tos-of-TI-Practice-1.pdf SAMHSA’s Trauma and Justice Strategic Initiative. (2014, July). SAMHSA’s Concept of Trauma and Guidance for a Trauma-Informed Approach. SAMHSA. https://store.samhsa.gov/sites/default/files/d7/priv/sma14-4884.pdf
Learning Objectives:
1. To elucidate the definition, ethos, and components of trauma-informed care practice to persons working in the healthcare industry and patients receiving care
2. To encourage individuals working in the healthcare industry to adopt trauma-informed care practice throughout healthcare institutions in order to increase patients’ feelings of safety while receiving healthcare
Patricia McGaffigan - Strengthening our Resilience - Implementation of Safer Together: A National Action Plan to Advance Patient Safety
Commitment and action is critical to achieving the goal of zero harm in health care. Despite substantial effort over the past 20 years, preventable harm in health care remains a major challenge concern in the United States.
Reliable implementation of the Safer Together: A National Action Plan to Advance Patient Safety — the “total systems safety bundle” — is essential for organizations to meaningfully reset and advance safe, reliable, and equitable care and to strengthen the resilience of systems. The National Action Plan (NAP), developed by 27 national organizations, provides leaders with an opportunity to candidly assess the current state of their organization’s foundational safety practices. It offers actionable solutions for a clear path forward to recover from setbacks that occurred during the pandemic and to advance and sustain the positive gains based on lessons learned over two decades of systems safety improvement work.
This session will focus on the four foundational areas of the NAP: Governance/Culture/Leadership, Patient & Family Engagement, Workforce Safety and Learning System, each with recommendations to advance specific elements that lead to a total systems approach to patient safety. Participants will be provided with an overview and instructions to complete the self-assessment. Tied together with the patient and family perspective, key insights will be shared by on behalf of health system leaders who championed the completion of the NAP Self-Assessment Tool and how it served not only as an exercise in scoring specific elements, but opened the door to necessary conversations to advance in patient safety. Strengthening the foundation for safety is no longer a choice — it is a leadership imperative. The National Action Plan is our path forward.
Learning Objectives:
1. Describe the four foundational areas essential to create total systems safety that are the center of the National Action Plan to Advance Patient Safety.
2. Describe actions to prompt significant advances toward total systems safety and safer care across the continuum of care.
David Birnbaum, Ph.D. and Dr. Naz Havaei - Learning from Things that Worked & Things that Didn’t: How Future Patient-Care Quality and Safety Programs Should be Structured to Survive Challenges and Leadership Change.

David Birnbaum, Ph.D., Adjunct Professor for the School of Population & Public Health at the University of British Columbia
David is self-employed on Vancouver Island and has decades of experience working as a hospital epidemiologist and infection control practitioner in the United States and Canada. Following employment by hospitals, he developed knowledge-based software products for the hospital epidemiology market, worked as an independent consultant to various professional and government organizations, and from 2008-2014 served as inaugural Program Manager for the Washington State Department of Health’s Healthcare Associated Infections Program. During academic appointments at several universities, he created courses in epidemiology, microbiology, research methods, statistics, management and quality improvement for professionals in nursing, public health, infection control, health care quality improvement, hospital epidemiology, public and business administration. Principal interests include surveillance methodology, infection control, quality assurance and improvement methods, health informatics, and self-directed (case/problem-based & distance) learning. His research and other publications have appeared in epidemiology, microbiology, governance and quality improvement journals. As a former member of the Society for Healthcare Epidemiology of America (SHEA), he served as its designated liaison to the Health Care Division of the American Society for Quality (ASQ) and chaired an international, interdisciplinary SHEA/ASQ-HCD Health Care Quality Improvement Special Interest Group. David also was a section editor for two SHEA journals; a contributing editor then regional editor for Emerald’s international journal Clinical Governance; senior co-editor for Emerald’s International Journal of Health Governance; and has served as a reviewer and editorial board member for several journals.

Dr. Naz Havaei, PhD, RN Assistant Professor of Nursing at the University of British Columbia
Dr. Havaei is a registered nurse, an assistant professor of nursing at the University of British Columbia, a health system researcher and a Michael Smith Health Research BC Scholar (2021-2026). Dr. Havaei has a passion for exploring and addressing workplace and policy factors that enable healthy outcomes for providers, patients and healthcare organizations. She is recognized as an emerging leader in health system research and has contributed to policy, practice and media platforms that support knowledge mobilization and research impact. To date, Dr. Havaei’s program of research has received $7 million in funding support from local, provincial and national funding agencies as primary investigator, resulting in over 40 peer-reviewed publications and over 50 conference presentations. Dr. Havaei teaches nursing leadership at the undergraduate and graduate levels.
Tejal Gandhi, MD - Emerging from COVID: Re-Energizing our Approach to Achieving Zero Harm

Tejal Gandhi, MD, MPH, CPPS, Chief Safety and Transformation Officer at Press Ganey
Tejal Gandhi, MD, MPH, CPPS, is the Chief Safety and Transformation Officer at Press Ganey. In this role, she is responsible for advancing the Zero Harm movement, improving patient and workforce safety, and developing innovative health care transformation strategies. In addition, Dr. Gandhi is leading the Press Ganey Equity Partnership to advance equity in health care. Before joining Press Ganey, Dr. Gandhi served as Chief Clinical and Safety Officer at the Institute for Healthcare Improvement (IHI), where she led IHI programs focusing on improving patient and workforce safety. Prior to this, Dr. Gandhi was President and Chief Executive Officer of the National Patient Safety Foundation (NPSF) from 2013 until 2017, when NPSF merged with IHI. She has also served as President of the Lucian Leape Institute, a think tank founded by NPSF that now operates within the IHI Safety portfolio and was a board member of the Certification Board for Professionals in Patient Safety which administers the Certified Professional in Patient Safety credential. Throughout her career, Dr. Gandhi has been committed to educating other clinicians on the topic of patient safety. She has been an invited speaker for numerous organizations nationally and internationally, has mentored physicians in post-doctoral study, and has frequently served on national and committees and boards. She is also a Certified Professional in Patient Safety. In 2019, Dr. Gandhi was elected as a member of the National Academy of Medicine. She is a recipient of the John M. Eisenberg Patient Safety and Quality Award, given in recognition of her contributions to understanding the epidemiology of medical errors in the outpatient setting and for developing prevention strategies. Dr. Gandhi has been named as one of the “100 Most Influential People in Healthcare,” “Top 25 Women in Healthcare,” “Top 25 Diversity Leaders in Healthcare” and “50 Most Influential Clinical Executives” by Modern Healthcare magazine. An internist by training, Dr. Gandhi previously served as Executive Director of Quality and Safety at Brigham and Women’s Hospital and as Chief Quality and Safety Officer at Partners Healthcare. She received her MD and MPH degrees from Harvard Medical School and the Harvard T.H. Chan School of Public Health and trained at Duke University Medical Center.
Panel Discussion - The landmark Federal legislation that would establish a National Patient Safety Board (NPSB)

Marty Hatlie, J.D, CEO, Project Patient Care (PPC), co-developer of the H2Pi – Healthcare & Patient Partnership Institute, and President of Partnership for Patient Safety.
Marty Hatlie is a patient safety advocate with a strong interest in the roles patients and family members play as co-creators of solutions. He currently serves as President & CEO for Project Patient Care, a Chicago-based nonprofit dedicated to engaging the voice and lived experience of diverse patients in healthcare improvement. In 2021 he co-founded Patients for Patient Safety US, a US branch of the World Health Organization’s Patients for Patient Safety network. PFPS US advocates implementation of the WHO Global Patient Safety Action Plan in the US. Hatlie is a former litigator, with a background in civil rights and medical liability defense work early in his career. In the 1980s and early 90s he was a lobbyist for the American Medical Association. Hatlie coordinated the AMA’s launch of the National Patient Safety Foundation in 1997 and served as its founding Executive Director from 1997—99. He is active in federal healthcare transformation work and currently serves on the National Steering Committee overseeing implementation of Safer Together: A National Action Plan to Advance Patient Safety.

Lisa McGiffert, Co-founder & Board President, PSAN (Patient Safety Action Network)
Since 2003, Lisa McGiffert has been a leading consumer/patient spokesperson on the prevention of medical harm. In 2018, she co-founded the Patient Safety Action Network, a national nonprofit coalition of advocates, including people who have been medically harmed. This patient led, patient driven network focuses on creating safer health care through accountability and transparency, with a focus on changes in state and federal policies. In 2022, she co-authored two reports on the failure of state medical boards to adequately communicate to the public about dangerous doctors. Her additional areas of expertise include accountability for hospital safety, FDA oversight of medical devices and prevention of health care acquired infections. Lisa previously led Consumer Reports’ Safe Patient Project, which among other successes, developed and worked to pass public hospital acquired infection reporting in 30 states. She has served on many national expert panels and committees that include developing evidence-based measures for patient safety, creating a framework for responding to infection outbreaks and serving as PSAN’s liaison to CDC’s infection advisory committee. McGiffert is frequently quoted in local, state and national media. She has received numerous recognitions, including Becker’s 50 experts leading the field of patient safety and Modern Healthcare’s 100 Most Influential People in HealthCare.

Helen Haskel, MA, Founder, Mothers Against Medical Error and President of Consumers Advancing Patient Safety
Helen Haskell is a longstanding US patient safety advocate with the nonprofit patient organizations Mothers Against Medical Error and Consumers Advancing Patient Safety. She is an Institute for Healthcare Improvement senior fellow, a board member of the Patient Safety Action Network and the International Society for Rapid Response Systems, and a previous chair of the WHO Patients for Patient Safety Advisory Group. Helen’s goal since the medical error death of her young son Lewis has been to enhance the patient contribution to safety and quality in healthcare. She has worked on policy at a state and federal level and served on many committees and research grants on patient safety and quality. She has written or co-authored dozens of articles, book chapters, and educational materials on patient engagement in safety and quality, including a co-edited textbook of case studies from the patient perspective. Her son Lewis’s story has been featured in educational programs and videos including Transparent Health’s full-length Lewis Blackman Story. Helen holds a bachelor’s degree in Classical Studies from Duke University and a master’s degree in Anthropology from Rice University.

Dr. Karen Feinstein, Ph.D., President and Chief Executive Officer of the Jewish Healthcare Foundation (JHF)
Dr. Karen Wolk Feinstein is President and Chief Executive Officer of the Jewish Healthcare Foundation (JHF) and its three operating arms, the Pittsburgh Regional Health Initiative (PRHI), Health Careers Futures (HCF), and the Women’s Health Activist Movement Global (WHAMglobal). Combined, they perform a unique mix of grantmaking, research, teaching, coaching, and project management to serve as a regional catalyst for healthcare reforms. Under her leadership, JHF and PRHI have become a leading voice in patient safety, healthcare quality, and related workforce issues. When Dr. Feinstein founded PRHI, it was among the nation’s first regional multi-stakeholder quality coalitions devoted simultaneously to advancing efficiency, best practices, and safety. Dr. Feinstein founded HCF to assist the region’s healthcare industry in attracting, preparing, and retaining employees. WHAMglobal was established to empower women to lead efforts to advance healthcare systems that are transparent, respectful, accountable, and equitable.
Panel Discussion - The Washington Patient Safety Speak-Up Award Winners discuss their experience of speaking up for safety.

Dani Morton, OB Surgical Technologist at University of Washington Medical Center.
Prevented an unintentionally retained foreign object through professional persistence.
Julia Ganey, Clinical Staff Pharmacist, Providence Swedish Cherry Hill Campus
For speaking up to identify areas of improvement in the identification and treatment of heparin induced thrombocytopenia (HIT) that resulted in multi-disciplinary education and changes in workflow.
Miranda Todd, RN, Harborview Medical Center
Miranda spoke up and advocated for immediate triage by the stroke team, rather than acquiesce to a decision for additional diagnostic interventions.
Sara Kim, Ph.D. - Tuning in to Prevent Harm: The Art of Impeccable Listening

Dr. Sara Kim, Ph.D., Research Professor of Surgery, Associate Dean for Educational Quality Improvement, University of Washington
Dr. Sara Kim, Research Professor of Surgery, received her PhD in Education in 1999 from University of Washington, Seattle, Washington. Currently, she serves as Associate Dean for Educational Quality Improvement, School of Medicine, University of Washington. Dr. Kim is the inaugural holder of the George G. B. Bilsten Professorship in the Art of Communication with Peers and Patients. She actively leads research programs in conflict management and collaborates with a wide range of clinical, administrative, and educational stakeholders across UW Medicine. Since 2014, she and her team have developed training programs and taught over 10,000 healthcare professionals conflict dialogue and speaking up skills. Her work has been primarily supported through the Arnold P. Gold Foundation Humanism in Medicine grants and the UW Medicine Patient Safety Innovation Programs (PSIP). She has numerous peer-reviewed publications in leading medical education and medical specialty journals, covering topics of communication skills for resolving conflict and negotiating power hierarchy. She is a certified coach for emerging and established leaders and a certified mediator for the King County Dispute Resolution Center in the State of Washington.
Mark Matthew and Meghann Brinoni - Transformative Change in British Columbia: Advancing Cultural Safety and Relationship Based Approaches to Healing

Mark Matthew, Director, Indigenous Health, Ministry of Health, Government of BC
Mark Matthew is Director, Indigenous Health, Ministry of Health, Government of BC. Mark grew up on the reserve of the Simpcw First Nation near Barriere, B.C. and has observed the consequences of colonization in his family, friends, and community. He continues to reflect on his unearned privilege of a white presenting male due to mixed parentage. Mark’s career in health began in 2007. After nearly a decade working in engagement, he moved to a new Quality team at FNHA in 2019 as the Manager of Quality Initiatives and Partner Relations. This work has given him the opportunity to explore various opportunities for change across the health system. In 2021 and 2022 he spent 10 months on secondment with the Ministry of Health to support the ‘In Plain Sight’ report recommendations, which provides guidance for change and the need for extensive reflection and humility throughout the health care system. In September 2022, Mark began with the BC Health Quality BC for a new opportunity as the Direction of Indigenous Health. Currently Mark lives on Tk’emlúps te Secwépemc (Kamloops) with his wife and two kids.
Meghann Brinoni, Executive Director, Indigenous Health and Reconciliation, Ministry of Health, Government of BC
Meghann Brinoni is an Executive Director, Indigenous Health and Reconciliation, Ministry of Health, Government of BC. Meghann began her career as a clinician in mental wellness and substance misuse at Interior Health and with First Nations across Secwepemc, Tsilhqot’in, and Dakelh territory. Later she conducted research related to mental wellness and land based approaches to healing. In 2014, Meghann joined First Nations Health Authority (FNHA) as the Manger of Research, Knowledge Exchange and Evaluation and in 2018 became the first Director of FNHA’s Quality department. Meghann resides in rural Northern Secwepemc territory and her passion is health systems improvement.
Patricia McGaffigan - Strengthening our Resilience - Implementation of Safer Together: A National Action Plan to Advance Patient Safety

Patricia McGaffigan, President of Certification Board for Professionals in Patient Safety, and Vice President at the Institute for Healthcare Improvement
Patricia is President, Certification Board for Professionals in Patient Safety, and Vice President, Safety at the Institute for Healthcare Improvement, where she leads a portfolio of patient and workforce safety and wellbeing initiatives. She is senior sponsor for the IHI’s Lucian Leape Institute and serves as Co-chair of the National Steering Committee for Patient Safety. Prior to the merger with IHI, Patricia was Chief Operating Officer, Senior Vice President of Safety Programs, and Interim President at the National Patient Safety Foundation. Her prior experience includes diverse roles in clinical practice, academia, and in start-up and established medical device companies focused on safety monitoring and clinical decision support. Patricia is a Certified Professional in Patient Safety (CPPS), a graduate of the AHA-NPSF Patient Safety Leadership Fellowship Program and serves on numerous national committees, taskforces, and technical expert panels, including the Joint Commission National Patient Safety Committee, the Joint Commission Journal on Quality and Patient Safety Editorial Advisory Board, the Advisory Committee of the Coalition to Improve Diagnosis, and the Partners for Nurse Staffing. Patricia is a Board Member of the Massachusetts Coalition for the Prevention of Medical Errors, the Foundation to Advance Nursing in Massachusetts, and Planetree’s Person-Centered Certification Committee. She is the recipient of the American Association of Critical Care Nurses Lifetime Member Award, the University of North Texas Health Science Center’s Mary E. Luibel Distinguished Service Award. and was named to Becker’s Review List of Patient Safety Experts to Know in 2023. Patricia received her BS in Nursing from Boston College and her MS in Nursing from Boston University.
Anna Kristina Moroz, Ph.D. - The promotion of trauma-informed care practice in medical settings

Dr. Anna Moroz, Ph.D.
Dr. Anna Moroz finished her PhD in linguistics at the University of Washington in 2021. Soon after, she had a traumatic wisdom tooth surgery where the staff made her feel extremely unsafe while preparing her for the procedure. While receiving medical care for PTSD like symptoms and extreme pain radiating from her jaw, she learned about trauma-informed care practice. She received a significant amount of closure for the traumatic event by discussing it and trauma-informed care practice with the surgeon. Since then, she has been able to build a supportive medical team but has also interacted with some providers who re-traumatized her. She has responded to those events by attempting to advocate for trauma-informed care at those facilities with mixed results. Feeling frustrated by her medical trauma history and feelings of unsafety interacting with medical providers, she wants to spread the tenets of trauma-informed care with the goal of being able to call any healthcare facility and ask for trauma-informed care providers so that her medical needs are met.
Patrick Neumann - New computer models reveal the drivers of nurse workload, missed care, and other quality threats in healthcare systems.

Dr. W. Patrick Neumann, Lic.Eng., LEL, Eur.Erg
Dr. W. Patrick Neumann, Lic.Eng., LEL, Eur.Erg. is a Design Scientist, a certified human factors professional and he heads the Human Factors Engineering Lab in Toronto Metropolitan University’s Department of Mechanical and Industrial Engineering, where he is Full Professor. He has published over 270 conference and scientific journal publications in the area of human factors in work system design with the intent of achieving sustainably superior workplaces that provide outstanding system quality and performance. Dr. Neumann’s work has been recognized internationally with “Best paper” awards in the biomedical, industrial engineering, and ergonomics literatures.
Harjinder Sandhu - Artificial Intelligence: improving the patient-provider experience in healthcare

Harjinder Sandhu, PhD, CTO, Health and Life Sciences, Microsoft
Harjinder Sandhu is the Chief Technology Officer, Health and Life Sciences at Microsoft. Harjinder is a serial entrepreneur in the healthcare technology space and has stood at the forefront of innovations in speech recognition and machine learning for more than 20 years. Earlier in his career, Harjinder co-founded MedRemote, a healthcare-focused speech recognition company acquired in 2007 by Nuance. He then served for five years as Vice President and Chief Technologist of Nuance’s Healthcare R&D division. He also co-founded the patient engagement company, Twistle, and remains on its Board of Directors. Harjinder holds a doctoral degree (Ph.D.) and master’s degree (M.Sc.) in Computer Science from the University of Toronto and a bachelor’s degree (B.Sc.) in Computer Science from The University of British Columbia. He is a former Assistant Professor of Computer Science at York University and Visiting Scientist at IBM.
Karthik Sivashanker, MD - Operationalizing Racial Justice and Equity in Health Care

Karthik Sivashanker, MD, MPH, CPPS is a nationally recognized expert and pioneer in the field of Quality, Safety and Equity. He currently serves as Vice President of Equitable Health Systems at the American Medical Association (AMA), and as a practicing psychiatrist at the Justice Resource Institute.
With a background that includes a Harvard Medical School Fellowship in Patient Safety and Quality, as well as a master’s in public health from the Harvard T.H. Chan School of Public Health, Dr. Sivashanker is committed to driving racial justice and equity in health care.
At Brigham and Women’s Hospital (BWH), Karthik became the first recognized Medical Director in Quality, Safety, and Equity in the country. As a clinical scholar at the Institute for Healthcare Improvement (IHI), he led a pivotal partnership with BWH to develop a groundbreaking system-wide model that integrates equity as a core strategy and embedded feature of strong quality and safety science and improvement work. He coined this “equity-informed high-reliability” framework as a critical approach for identifying and addressing inequities that were previously hidden and differentially harming patients, staff, and communities.
Since joining the AMA, Karthik has emerged as a national thought leader, spearheading initiatives to fundamentally transform health care to achieve optimal health outcomes for every person and community. His team launched the Peer Network for Advancing Equity through Quality and Safety, a first-of-its-kind collaboration led by the AMA in partnership with The Joint Commission and BWH. Through this program, Karthik has successfully spread awareness and accelerated adoption of an integrated model for quality, safety, and equity to other health systems across the country. It has subsequently led to the formation of a Quality Safety and Equity network, comprised of a critical mass of leaders and organizations working together to advocate, share, learn, and innovate to address real-time harms and opportunities.
Karthik is also a key architect of the Rise to Health Coalition, a prominent national initiative bringing together individuals and organizations for coordinated action and collective impact for equity. Co-led by Karthik and supported by key partners, the Coalition is focused on building capacity, influence, and momentum for change in four key impact areas: access, quality and safety, workforce, and social and structural drivers of health. Recognizing the critical importance of sustainably changing mindsets and narratives within health care around equity and racial justice, Karthik and his team designed and launched the National Health Equity Grand Rounds. This free educational series features fiery panel conversations with leading voices and diverse thinkers as they grapple in real time with complex and urgent issues. The inaugural event, “History of Racism in U.S. Health Care: Root Causes of Today’s Hierarchy and Systems of Power” featured Harriet A. Washington, author of Medical Apartheid, and was viewed live by over 4500 attendees. As overall leader for health equity education in the Center for Health Equity, Karthik and his team are actively reshaping the field of medical education by developing high-quality health equity curricula across a range of topics and types of learners.
Karthik has been repeatedly engaged for his expertise via national advisory and technical panels with a focus on improving healthcare practices and policies at both the state and national levels, such as The Joint Commission, the Centers for Medicare and Medicaid Services, the CDC, and the Presidential COVID-19 Health Equity Task Force. He has participated in numerous media conversations where he has consistently emphasized the critical relationship between equity, quality, and safety in healthcare. His contributions range from a Harvard Business Review webinar on using data to address racial inequities (September 2022) to participating in an Atlantic Roundtable conversation with other invited health equity leaders (April 2023). He has also been featured in podcasts and interviews with organizations such as the CDC and NEJM, where he addressed topics like equitable infection prevention control, dismantling racism in healthcare, and advancing safety and equity. His work to address differential COVID-19 impacts for Latinos was by covered by NPR news.
As a former Fulbright scholar, he conducted groundbreaking research on the vertical transmission of HIV/AIDS in rural Venezuelan mountain communities. As a VA Under Secretary for Health Diffusion of Excellence Gold Fellow, he led work to standardize and improve substance use screening and triage for Veterans. He is a devoted father, a talented musician, a fierce advocate, and a loyal friend.
Umair A. Shah, MD, MPH, Secretary of Health, Washington State - Opening Keynote

Umair A. Shah, MD, MPH, Secretary of Health, State of Washington
Umair A. Shah, MD, MPH, is the Secretary of Health for the great state of Washington, appointed by Governor Jay Inslee in December 2020. He is the first Asian-American physician of South Asian descent to serve in this leadership role in the history of Washington, home to nearly 8 million people. Dr. Shah earned his BA (philosophy) from Vanderbilt University; his MD from the University of Toledo Health Science Center; and completed an Internal Medicine Residency, Primary Care/General Medicine Fellowship, & MPH (management), at the University of Texas Health Science Center in Houston. He also completed a global health policy internship at World Health Organization headquarters in Switzerland. Over his career, Dr. Shah has been a clinician, innovator, educator, and leader in health. He has been a champion for underserved communities, at the intersection of health and health care, while charting a fresh course in health by centering on the cornerstone values of equity, innovation, and engagement.
Saul Weingart, MD - Finding the Patient in Patient Safety
Saul Weingart, MD, Professor of Medicine at Brown University’s Warren Alpert School of Medicine
Dr. Weingart holds a doctorate in public policy from Harvard University and an MD degree from the University of Rochester. He served as VP for Quality Improvement and Patient Safety at Dana-Farber Cancer Institute from 2004-13, Chief Medical Officer and SVP of Medical Affairs at Tufts Medical Center from 2013-21, and as President of Rhode Island Hospital and Hasbro Children’s Hospital from 2021-23. He is currently Professor of Medicine at Brown University’s Warren Alpert School of Medicine. Dr. Weingart is a practicing general internist. He has published extensively on topics that include patient safety in primary and specialty care; opportunities and limitations of patient engagement in patient safety; strategies to understand and enhance patient, family, and clinician error reporting; quality measurement; and diagnostic errors. Dr. Weingart served as chair of the board of governors and as a director of the National Patient Safety Foundation and on various editorial and advisory boards. He is the recipient of the 2012 John M. Eisenberg individual achievement award in quality and patient safety.
Stefan Wheat, MD - Navigating the Nexus: Examining the Interplay Between Patient Safety, Quality, and Climate Change in Healthcare
Stefan Wheat, MD, Emergency Physician & Faculty at the University of Washington
Stefan Wheat, MD is an Emergency Physician and faculty in the Department of Emergency Medicine at the University of Washington. With the Center for Health and the Global Environment (CHanGE) at the University of Washington, Dr. Wheat works to understand the scope of the health threats posed by climate change, promote healthcare system adaptation and emergency preparedness, and inform policies to keep people safe in a rapidly changing world. He completed a fellowship in Climate & Health Science Policy at the University of Colorado where he worked as a Physician-Fellow at the Department of Health and Human Services in their Office of Climate Change and Health Equity (OCCHE) and as an Associate Research Scientist at Columbia University’s Global Consortium on Climate and Health Education. His work has included founding ClimateRx, a seamless tool designed to help health professionals to connect with patients and colleagues on how we can respond to the health risks of climate change, and the development of Climate Resources for Health Education (CRHE), a global health professional-led initiative that aims to provide free, publicly accessible, evidence-based resources to accelerate the incorporation of climate change and planetary health information into educational curricula.
We are pleased to invite interested sponsors to support our 20th annual conference. As a sponsor you are helping to subsidize the cost of the conference to healthcare staff and provide free attendance to patients, families, and students.
THIS YEAR’S PACKAGES OFFER SEVERAL LEVELS FROM WHICH TO CHOOSE.
Details of package benefits are described in the application.
- Platinum Sponsor – $10,000 (1 available)

- Gold Sponsor(s) – $7,500 (3 available)
- Silver Sponsor(s) – $5,000
- Bronze Sponsor(s) – $2,500
- Supporter(s) of Patient Safety – $1,500
All sponsors will be recognized on the Washington Patient Safety Coalition website and marketing materials with sponsor logos linking to a webpage of your choice.
Platinum, Gold, Silver and Bronze sponsors have access to a dedicated page on the conference website which can include images, videos, links, etc.
Downloadable PDF version here: AGENDA
DAY 1 – Tuesday, October 17, 2023 8:00 A.M. - 1:00 P.M. (PST)

DAY 2 – Wednesday, October 18, 2023 8:00 A.M. - 1:00 P.M. (PST)

WELCOME TO THE 2023 20TH ANNUAL NORTHWEST PATIENT SAFETY CONFERENCE!
For those who were able to attend the live conference, we hope you enjoyed it and learned plenty!
If you were not able to attend the live conference, do not worry, we will be uploading the conference sessions in the event portal on November 6. To gain access to the portal and watch the sessions, you will be required to enter your attendee confirmation code. You can find your code at the very bottom of your registration confirmation email or by clicking HERE and entering your email to get it resent. If you continue to have trouble getting in, please contact Steve Levy at 206-204-7383 or Amelina Kassa at 206-204-8384.
C.E. Credit Information:
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2023 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. For CE credits go directly to question 12. However, we encourage you to complete the entire survey and provide us with feedback! Upon receipt of your survey/CE application, we will either send you a certificate(s) or for CNEs we will send you a required questionnaire about each presentation.
RECORDED PRESENTATIONS:
The conference presentations will be posted on the conference event portal on November 6. To view the recorded presentations, log into the event portal at the “enter event portal here” button above and enter your attendee confirmation code (you can find your attendee confirmation code at the very bottom of your registration confirmation email or by clicking HERE and entering your email to get it resent.) Once you are logged into the portal, click on the “General Info” tab at the top of the page. The presentations, slides, and supporting materials will all be posted here sorted by presentation date and time.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
In the event portal, toward the top of the “General Info” page is a section called “How to get educational credits.” In this section is a link to a CE application form used for the recordings. Use this for all recorded presentations. Upon receipt of your CE application, we will send you the certificate(s).

ART SPEAKS
For the second year, WPSC’s Addressing Stigma & Bias Workgroup is featuring artwork as a powerful way to connect with patients’ experiences with health conditions. Our focus this year is mental illness & behavioral health.
Art is not only beautiful, it is a potent medium of expression. Evocative and compelling, it touches the soul and connects in a way no other medium can.
Featured artwork this year include art and a poem by PNW residents Louie Gong, Mahvish Naqvi, Munira Leslie Sinclair and Anita Sulaiman as well as a poem by model-turned actress and mental health advocate, Cara Delevingne. Big thank you to the artists for sharing their compelling pieces with us.
**************************************************************************************************************************************************************************
Visual Art
**************************************************************************************************************************************************************************

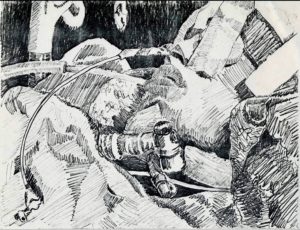
ART PIECE: Black Sheep
Click here for a video showing the making of this piece
ARTIST NAME: Louie Gong
Click here for artist’s biography and link to Eighth Generation.
ARTIST INFO: Louie Gong (Nooksack) is the founder of Eighth Generation. A self-taught artist who was raised by his grandparents in the Nooksack tribal community in northwest Washington, he got his start by painting cultural art on shoes.
Realizing that creating one-of-a-kind pieces did not provide a sustainable pathway to success, he began applying his artwork to accessibly priced products. His unique style merges traditional Coast Salish art with influences from his mixed heritage and urban environment to create work that resonates widely across communities and cultures.
Black Sheep is about drawing power from past experiences— even traumas. It is about self-care.
“I’ve been thinking about the term baggage, and it’s all wrong. When we think about our past experiences as something we can just put down, we can’t actually heal. The real pathway to becoming stronger and more confident versions of ourselves is to learn to live in symbiosis with our past experiences.”
The Black Sheep’s body is composed of Louie’s signature wolf-mouth motif, which he uses here to symbolize negative past experiences. It is painted loosely to indicate the frequent movement of and the idea that our past experiences are living parts of us that we can’t simply set down as if they were “baggage.”
By contrast, the Black Sheep’s face is composed of highly structured Coast Salish design elements to indicate the self-confidence drawn from the understanding that past experiences make us better equipped to manage whatever lies ahead. A few understated sprouts indicate constant growth regardless of what we are experiencing.
__________________________________________________________________________________________________________________
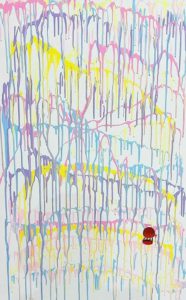
ART PIECE: Bleed Joy
ARTIST NAME: Tahira Naqvi
ARTIST INFO: I am a new artist venturing out to create artwork that speaks to mental health struggles. Childhood trauma is a big factor in my art, which is abstract and comes from the heart. It delves into deep wounds and the quest to achieve joy through self-reflection. I speak through colors and shapes that represent this journey of self-healing.
When I started on this piece, I did not know what to create, but I knew I wanted to display my pain, my joy, and my journey. So, I faced the canvas and decided to just let it flow. This piece has chaos, joy and a dark passenger. All representing the struggle between my child and adult selves. There is a hot air balloon. When I was little, I always wanted to escape. One day, I took my mom’s large shoe box and tied her red scarf to its four ends, after which, I walked out to our balcony and tried to leap off to go explore the world. Except, my grandfather saved me.
I have a natural instinct to leap forward and escape. It took cycles of anxiety to create this very personal piece. “Bleed Joy” is for everyone dealing with mental chaos and anxiety in their lives. My hope is that, by putting this out there, I will finally heal and find contentment.
_________________________________________________________________________________________________________________
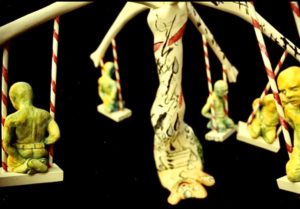
ART PIECE: Untitled
ARTIST NAME: Munira Leslie Sinclair
ARTIST INFO: Munira Leslie Sinclair was a talented visual artist, eloquent writer & devoted mother to her children, including an adult son with severe traumatic brain injury (TBI). Much of her artwork was inspired by her struggles through some very difficult times as well as the unrelenting challenges of trying to ensure quality care for her son with special needs, in a system not well set up for patients like him. A passionate patient advocate, she worked to improve the lives of those with TBI through legislation & advocacy training. While she faced adversity & bouts of cancer with fortitude, art was her outlet.
Leslie passed away on September 30, 2022. Special thanks go to her daughter, Jennifer, who has given WPSC’s Addressing Stigma & Bias Workgroup permission to share these 2 pieces with our audience.
**************************************************************************************************************************************************************************
Poetry
**************************************************************************************************************************************************************************
EVERYTHING CHANGES
Everything is touched
by the sea of time.
We are life forms
on the shore
of existence.
No matter how you try
to be immovable,
time moves you.
It caresses you,
lulls you,
embraces you.
Just as you’re buoyed
into a comfortable slumber,
it snatches you,
pulls you out
& swallows you.
It swirls you around
& sucks you in.
Then,
just as suddenly,
it floats you,
breathless,
onto its surface.
The winds of change
calm to a whisper.
You feel it
cushioning you,
as you lay
adrift
with your face to the sky.
Then it stirs,
picks you up,
carries you
on a wave;
pushes you forward,
races you
back to shore
& deposits you,
gently,
onto the sand.
Glistening in the sun,
you catch your ragged breath. And settle down.
Before long,
you’re feeling the breeze
on your face,
looking up at the stars
& thinking:
I could stay like this forever.
You inhale the stillness…
Then it wakes you
from your reverie.
It foams
at your feet,
kissing your toes,
nudging you.
It teases you
into motion.
Slowly,
you move to the tide’s rhythmic touch,
sway to its hypnotic gyrations
& join,
again,
the dance of life.
—
Tomorrow becomes today.
Today becomes yesterday. Yesterday is but a memory.
Did we remember to live in today?
© 2020 Anita Sulaiman
POEM TITLE: EVERTHING CHANGES
ARTIST NAME: Anita Sulaiman
ARTIST INFO: Anita Sulaiman is Principal Consultant and Executive Coach at IBEX Consulting, whose areas of expertise include strategy, leadership development, marketing and change management/business process re-engineering. Anita is also a culture coach specializing in cultural competency and cross-cultural communication. Helping individuals and organizations excel in a global world is a passion.
Anita stays at the forefront of efforts to improve patient safety, serving on advisory groups and committees for organizations including the Washington Patient Safety Coalition, Foundation for Health Care Quality (Patient & Family Advisory Council) and Washington State Coalition for Language Access. She is Chair of the Addressing Stigma and Bias Workgroup, a partnership between WPSC and the Bree Collaborative, a healthcare non-profit established by the Washington State Legislature.
Everything Changes was written at a time of emotional turmoil. In the midst of personal upheaval, thanks to the practice of meditation to help with her mental health, this poem about the vagaries of time captures moments of clarity from seeing that change, while invariably very stress-inducing, are part of the ebb & flow of life.
_________________________________________________________________________________________________________________
MOTHER
Mother
You are & you aren’t her
You’ve had to be mother & father
Did you know – you were the world to me?
Your eyes the window through which I see
Mother
Not a word to use in vain
So why are you my biggest source of pain?
You are the reason I am here
You are the idea I hold dear
What is this figure?
We call mother
What is this idea?
No other thing comes near
She is a hug
A warm embrace
Someone who’s there to kiss your face
To hold your hand
To wipe your tears
She’s there to chase away your fears
She is the reason
You stand strong
Can tell the difference between right & wrong
She is your shelter
From the storm
The well you get your reassurance from
At least that’s what
Everyone seems to think
They don’t know yours pushed you to the brink
Put you down
And cast you out
Always wished she could’ve done without
Mine gave me a bit of love
And a lot of hate
Served honey & poison on the same plate
Was never there
To kiss my face
But she made sure I always knew my place
I had no shelter
From storms or even rain
What I had
Would drive most people insane
There was no one
To wipe away my tears
I had someone filling my heart with fears
While you had hugs
Someone to hold your hand
I had to figure out where I stand
You always knew
Where you belong
All I was ever told was I was wrong
Wrong to want
To ask or to question
To live for others – that is my mission
You had wind beneath your wings?
Me?
Who am I to have needs or feelings?
While you had kisses
A friend & all
Someone to catch you when you fall
I had no right
To be happy
Yes, that was what she said to me
So don’t tell me
How I’m supposed to feel
You don’t know what for me is real
Don’t bother
To pile on the guilt
That’s the foundation on which I was built
All that said
Good comes with bad
She’s the only mother I’ve ever had
The person
Who instilled in me
All the good things that to this day you see
She taught me
Through trial by fire
How to prevail & always aim higher
Yes, I suffered
A million cuts
I also have the biggest heart of hearts
Mummy
If you only knew
All the love I have in my heart for you
To me
You gave birth
Yet for some reason
You don’t know my worth
I am
Pure love
A blessing
A gift from the Lord above
That is what babies are
Not a thing comes close
Not even by far
Today
I make peace
With all that was, will be & all that is
I can’t forget
But I forgive
You were only doing your best to live
In return
These things I ask
No more pretenses
Take off your mask
It’s time
Let go
Set yourself free
From who you think you’re supposed to be
I am trying
To do the same
Life is too short
For anger or for blame
I hope you see
That just like you
I am human
I’m doing my best too
All my life
Through all the hurts
I’ve been held to impossible standards
Now I know
It’s clear to me
Those high bars
Were what you were made to see
On this day
I hereby purge
I release
So we both can finally have peace
From here on
May we know
Acceptance
And a better tomorrow
Happy Mother’s Day.
© Anita Sulaiman 2023
POEM TITLE: MOTHER
ARTIST NAME: Anita Sulaiman
ARTIST INFO: Anita Sulaiman is Principal Consultant and Executive Coach at IBEX Consulting, whose areas of expertise include strategy, leadership development, marketing and change management/business process re-engineering. Anita is also a culture coach specializing in cultural competency and cross-cultural communication. Helping individuals and organizations excel in a global world is a passion.
Anita stays at the forefront of efforts to improve patient safety, serving on advisory groups and committees for organizations including the Washington Patient Safety Coalition, Foundation for Health Care Quality (Patient & Family Advisory Council) and Washington State Coalition for Language Access. She is Chair of the Addressing Stigma and Bias Workgroup, a partnership between WPSC and the Bree Collaborative, a healthcare non-profit established by the Washington State Legislature.
Mother’s Day is a tough one for me. This year, I struggled as I did in previous years. Except, this year, my mother, who recently turned 80, is very ill. Her condition has intensified for me all the emotions tied to her. This poem is dedicated to all who can relate.
Usually, the words just come. I have to scribble quickly & I am done. This time, I struggled. The words wanted to come out, but… Something in me resisted. I had to fight to let these truths out. To give them the light of day felt like giving my pain validity.
Writing down these words meant staring my trauma in the face. It meant ripping off the plaster. In the end, it was exactly what needed to be done. This is validation I needed to gift to myself. I am giving myself long overdue permission to feel, to acknowledge. It is what it is. No matter what people say, it’s ok. It’s not right, but it’s ok. With that realization comes release.
My poems are medicine to me. Sometimes they are light that shows the way – guidance from a place of pure love. Now I can start to heal, God willing.
This is my art; my outlet; expression from the deeper parts of me. This is my balm; my inspired remedy. This is healing for my soul. Poetry, for me, is all that & more. It’s my connection with the Divine. It is divine.
WHO AM I TRYING TO BE?
Who am I? Who am I trying to be?
Not myself, anyone but myself.
Living in a fantasy to bury the reality,
Making myself the mystery,
A strong facade disguising the misery.
Empty, but beyond the point of emptiness,
Full to brim with fake confidence,
A guard that will never be broken,
Because I broke a long time ago.
I’m hurting but don’t tell anyone.
No one needs to know.
Don’t show or you’ve failed.
Always okay, always fine, always on show.
The show must go on.
It will never stop.
The show must not go on,
But I know it will.
I give up. I give up giving up.
I am lost.
I don’t need to be saved,
I need to be found.
POEM TITLE: WHO AM I TRYING TO BE?
ARTIST NAME: Cara Delevingne
ARTIST INFO: Cara Delevingne, actress and model, shares her personal experiences with anxiety and depression.











