The 21st Northwest Patient Safety Conference
“Safe Patient Care: It Takes All of Us”
Focusing on what we can do together for safety
October 15th and 16th, 2024
Presented in collaboration with the Oregon Patient Safety Commission and Health Quality BC
The recorded conference sessions are now available!
Registration remains open if you missed the live event!
To register, please contact Amelina Kassa at akassa@qualityhealth.org.
HOW TO VIEW THE RECORDED PRESENTATIONS
The conference presentations are posted on the conference event portal. If you registered for the live conference, all presentations, and supporting materials, are available for you to view. To view the recorded presentations, log into the event portal just as you did for the live event using the link found in your registration confirmation and enter your attendee confirmation code (you can find your code at the bottom of your registration confirmation email or click HERE to have it resent to your email. If you encounter any issues accessing the portal, please contact Amelina Kassa for assistance.) Once you are logged into the portal, click on the “Info” tab at the top of the page (most left tab). The presentations, slides, and supporting materials will all be posted below on the page sorted by presentation date and time.
HOW TO REGISTER FOR THE CONFERENCE TO WATCH THE RECORDED PRESENTATIONS
Didn’t get to attend the live event? No worries, we’ve got you covered! To register, please contact Amelina Kassa at akassa@qualityhealth.org. Amelina will get you registered. Conference discounts apply through December 31, 2024! After that, discounts will end. See the registration tab for more information.
C.E. CREDIT INFORMATION:
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2024 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. Upon receipt of your survey/CE application, we will either send you a certificate(s) or for Nursing Contact Hours we will send you a required questionnaire about each presentation.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
To apply for credits, click here for the CE application form. Upon receipt of your CE application, we will send you the certificate(s). If you previously applied for live conference credits, please use the same personal information here so we may reconcile live and recorded applications. If you attended the live conference and didn’t submit an evaluation for CEs, use this evaluation for both live and recorded viewings.
Nursing Contact Hours: If you request Nursing Contact Hours, a follow-up conference evaluation is required by the California Board of Registered Nursing. Click here for the Nursing Evaluation. Upon receipt of your nursing evaluation, we will send you the certificate with your contact hours. If you only want Nursing Credit Hours, then you do not need to complete the conference evaluation.
ABOUT THE CONFERENCE
Welcome to our 21st conference! The theme is “Safe Patient Care: It Takes All of Us.” At its most basic level, health care boils down to one-on-one interactions between people. The conference will focus on what patients, residents and providers can do together to improve safety, quality, and outcomes. We have truly great faculty offering 14 hours of programming. Presentations will be recorded and available for a year for everyone registered. We’ve expanded our available CE credits: BCPA, CPHQ, CPHRM, CPPS and Nursing Contact Hours.
The conference keynote will be given by Danielle Ofri, MD, PhD. She is a primary care internist at Bellevue Hospital, the oldest public hospital in the country. She is Founder/Editor-in-Chief of the Bellevue Literary Review, and is a clinical professor of medicine at NYU School of Medicine. Danielle Ofri is the author of six books about life in medicine:
- When We Do Harm: A Doctor Confronts Medical Error
- What Doctors Feel: How Emotions Affect the Practice of Medicine
- Medicine in Translation
- What Patients Say; What Doctors Hear
- Incidental Findings
- Singular Intimacies: Becoming a Doctor at Bellevue
A SAMPLE OF PRESENTATION TOPICS
- Workforce civility: Explore the State of the Science related to civility, incivility, and other forms of workplace aggression and examine individual & organizational competencies to foster healthy, productive work environments.
- Restorative justice: Learn about the “Social Determinants of Trust” to build foundations for trust with patients, right from the start.
- Intersex management: Expand your understanding of patient safety when considering children’s rights and contemplate the meaning of medical harm in the context of pediatric genital surgeries.
- Cognitive interviewing: Learn about the role of investigative interviews in fact-finding, the cognitive interviewing protocol, and practical advice for the investigations in healthcare settings.
- Artificial intelligence: Discuss potential pitfalls of applying AI for clinical diagnosis without adequate guardrails. Learn the ethical and legal challenges around AI implementation in health care.
- Shared decision making: Learn how Massachusetts General Hospital built a culture of shared decision making to increase patient engagement. And discuss the challenges and facilitators for implementation of patient decision aids to enhance shared decision making from Confluence Health, University of Colorado and the University of Ottawa.
- British Columbia’s Patient Voices Network: Learn about a community of patients, families, and caregivers who team up with health care professionals to improve health care in BC. If you are a patient advocate, experience officer, manage or participate on a PFAC you’ll want to attend this.
- Long term care: Learn about long term care facilities that have an innovative staff-centered approach to quality improvement that results in staff with higher morale, better staff retention, fewer workplace injuries, falls and medication errors.
- Racism and medical education: Understand and identify systemic racism in health professions education and understand its impact on student experiences and patient quality and safety.
- Leapfrog’s national hospital ratings: We’ll pull back the curtain on Leapfrog’s methodology to access health care safety and discuss how patients, purchasers, hospitals, and others can use the published data.
About the Northwest Patient Safety Conference
Now in its 20th year, the Northwest Patient Safety Conference is the only event of its kind in the Western US, uniting healthcare professionals, providers, patients, families, and caregivers from all care settings for networking and engaging in sessions with industry thought leaders invested in improving the patient experience. This year’s conference is our second virtual conference, and our second year in collaboration between the Washington Patient Safety Coalition, the Oregon Patient Safety Commission, and Health Quality BC.
Members of the conference committee who are putting on this fantastic conference
Amelina Kassa Jo Sedman
Anita Sulaiman Naomi Kirtner
David Birnbaum Rex Johnson
Farinaz Havaei Rhonda Bowen
Jamie Leviton Valerie Harmon
Jeff Goldenberg Yanling Yu

TO REGISTER EMAIL
Amelina Kassa <akassa@qualityhealth.org>
This year’s conference is presented in collaboration with the Oregon Patient Safety Commission and Health Quality BC.
Conference Format: Virtual, you will receive a secure link to the conference presentations.
Dates and times: October 15 & 16, 2024
Total presentations: 14
- Healthcare professionals and anyone seeking continuing educational credits, $85
- Patients, their families, and healthcare profession students attend free
- Discounts are offered through December 31, 2024 for registrants with CPHQ, CPPS, CPHRM, and BCPA professional certifications.
Payments accepted: all major credit cards via PayPal.
Continuing educational credits: Attendees are eligible for Nursing Contact Hours, CPHQ, CPPS, CPHRM, and BCPA educational credits. These may be acquired by attending the live sessions or watching the recorded sessions up to the next conference in October 2025.
*Recorded educational credit availability is determined by the accrediting organization. Attendees will request CE credits via a conference survey following the conference or via a form on the recorded conference website. PLEASE NOTE THE CREDIT AMOUNTS MAY CHANGE IF THE AGENDA CHANGES.
| Credit Type | Total Credits for Conference | Credits Available for Recordings |
| BCPA | 3 JEDI 11 General Click here for Approved Program Content (live & recorded) |
Up to the 3 JEDI and 11 General
|
| CPHQ | 14 total available 8 for attending live |
Up to the 14 total |
| CPHRM | 14 total available 8 for attending live This meeting has been approved for a total of 14.0 contact hours of Continuing Education Credit toward fulfillment of the requirements of ASHRM designations of FASHRM (Fellow) and DFASHRM (Distinguished Fellow) and towards CPHRM renewal. |
Up to the 14 total
|
| CPPS | 14 total available 8 for attending live This activity meets the criteria of the Certification Board for Professionals in Patient Safety for up to 14.0 CPPS CE hours. |
Up to the 14 total
|
| Nursing Contact Hours | 16.8 total available 9.6 for attending live ”Provider approved by the California Board of Registered Nursing, Provider Number CEP 16359 for 16.8 contact hours.” |
Up to the 16.8 total |
Registration questions? Contact Amelina Kassa <akassa@qualityhealth.org>
Call Steve Levy, Executive Director, 206-204-7383
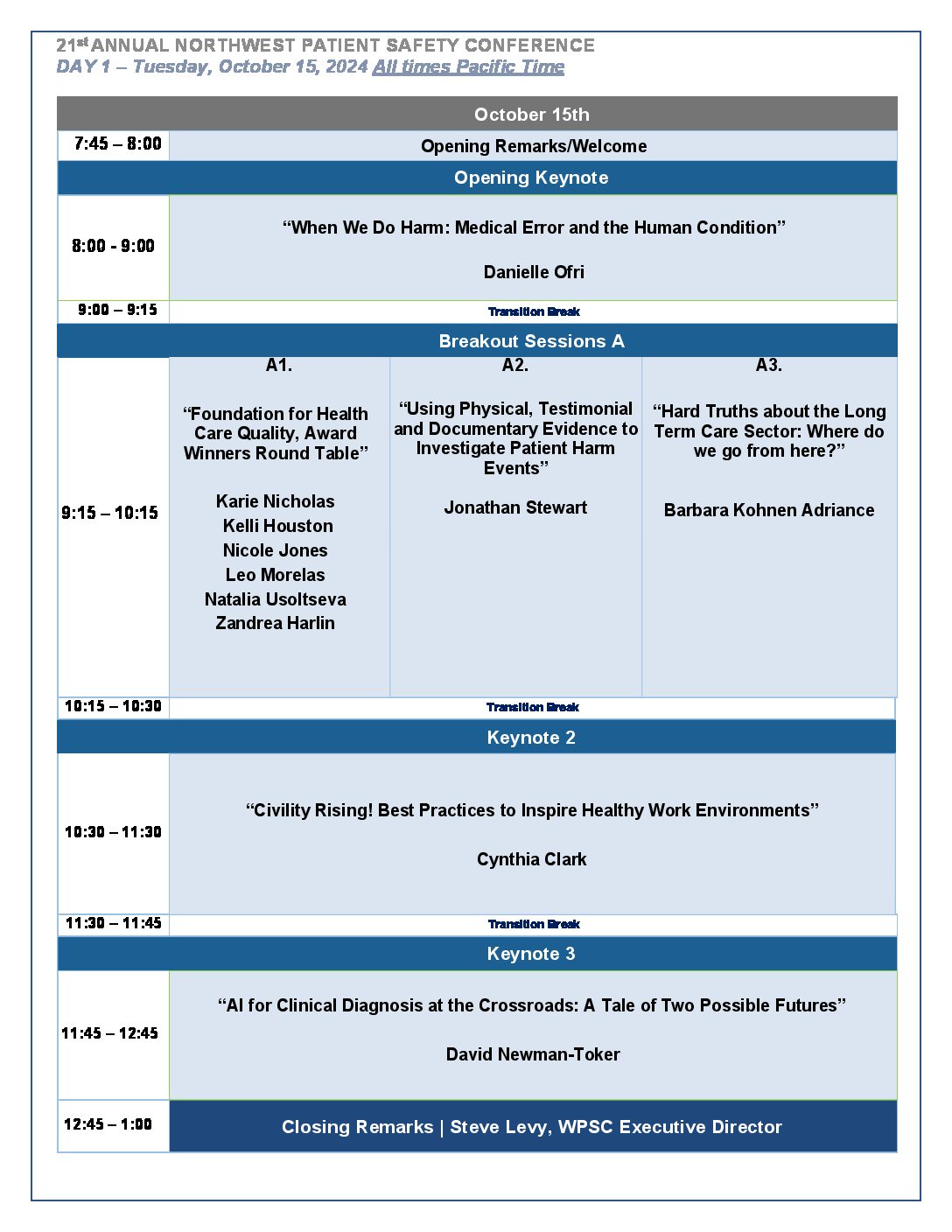
Opening Keynote: When We Do Harm: Medical Error and the Human Condition - Danielle Ofri
Patient safety is a critical issue in medicine today. There is, rightly, a strong emphasis on systems approaches to improving medical care and decreasing error. However, medicine is fundamentally a human endeavor. Without attention to the human aspects of the medical enterprise—emotions, cognitive abilities, biases, communication—crucial aspects of patient safety will remain beyond our grasp.
Learning Objectives:
- Describe how the culture of medicine can endanger the health and safety of patients.
- Explain the role of emotions, cognition, and communication regarding medical error.
- Identify opportunities to improve the delivery of care while navigating an imperfect health care environment.
Please note that Danielle Ofri does not use Power Point in her lectures. Technical requirements are only a microphone and a cup of tea.
A restorative approach to harm and preparing for uncertainty - Carolyn Canfield
Trust is assumed to be a pre-requisite for patients. However, trust may not sit comfortably with our concepts and practices in risk management, the actual experience of harm and the rocky recovery after harm. Carolyn Canfield will lead this discussion drawing on trust as a throughline in her personal experience with harm, her exploration of system resilience and restorative justice, and a decade of teaching patient safety to medical students.
Leaning Objectives:
- Explain how relationship-building with patients can affect the safety of care and management of risk.
- Compose “What’s One Thing…?” questions to open trust-building conversations and learn patient priorities.
- Apply a “Social Determinants of Trust” lens on building foundations for trust with patients, right from the start.
AI for Clinical Diagnosis at the Crossroads A Tale of Two Possible Futures - David Newman-Toker
Most diagnostic errors are associated with issues in bedside diagnostic reasoning and appear to disproportionately reflect failures of clinical expertise, which has the potential to be addressed by AI. Before us lie two possible paths: one in which AI promotes diagnostic excellence and the other in which AI promotes efficiency but sacrifices quality and safety. In this session, we will explore what it will take to achieve the more desirable future—a world where diagnoses are accurate, timely, and effectively communicated to patients, avoiding both diagnostic error and overdiagnosis… one where diagnostic processes are patient-centered, evidence-based, prompt, efficient, safe, and equitable.
Learning Objectives:
- Summarize public health burden & financial impact of diagnostic errors and misdiagnosis-related harms.
- Discuss potential pitfalls of applying artificial intelligence (AI) for clinical diagnosis without adequate guardrails.
- Describe prerequisites and systems of care essential to deploying AI to achieve diagnostic excellence.
Artificial Intelligence and health care: Its applications and hidden dangers - Sian Hsiang-Te Tsuei
The presentation discusses ethical and legal challenges around artificial intelligence implementation in health care using various types of AI software designs and cutting-edge AI-related health care applications as examples.
Learning Objectives:
- Define artificial intelligence.
- Recognize opportunities around how AI can improve health care service delivery.
- Recognize potential ethical and legal threats around AI implementation.
Civility Rising! Best Practices to Inspire Healthy Work Environments - Cynthia Clark
The detrimental impact of workplace incivility is well documented, and if allowed to take root, the consequences can be serious. So, imagine an enjoyable workplace—an environment where you and your colleagues can truly thrive in your career and profession. This engaging and thought-provoking session provides a deepened and empirical understanding of workplace incivility, its impact on individuals, teams, organizations, and patient care—and emphasizes ways to build and sustain healthy work environments. Join a renowned nurse researcher, award-winning professor, and accomplished author for a stimulating session to explore best practices to foster healthy, vibrant work environments.
Learning Objectives:
- Explore the State of the Science related to civility, incivility, and other forms of workplace aggression.
- Describe the impact of incivility on individuals, teams, organizations, and patient care.
- Examine individual & organizational competencies to foster healthy, productive work environments.
Selected References
Access to Dr. Clark’s empirical measurements, theoretical models, and reflective assessments can be obtained by browsing her Civility MattersTM website and scrolling to the Licensed Works link. Participants may be interested in Dr. Clark’s most recent book, Core Competencies of Civility in Nursing & Healthcare—a must-read for all nurses and health care professionals which details evidence-based strategies to foster civility and healthy work environments. There is an ancillary facilitator guide and learner workbook associated with the book. The much anticipated 3rd edition of her book, Creating and Sustaining Civility in Nursing Education: A Faculty Field Guide is scheduled to be released spring 2025.
- Brassey, J., Herbig, B., Jeffery, B., & Ungerman, D. (2023). Reframing employee health: Moving beyond burnout to holistic health, McKinsey Health Institute, https://www.mckinsey.com/mhi/our-insights/reframing-employee-health-moving-beyond-burnout-to-holistic-health
- Clark, C.M. (2022). Core competencies of civility in nursing & healthcare. Sigma.
- Clark, C.M, Gorton, K., & Bentley, A. (2022). Civility: A concept analysis revisited, Nursing Outlook. 70(2), 259-270. https://doi.org/10.1016/j.outlook.2021.11.001
- Clark, C.M. Landis, T., Barbosa-Leiker, C. (2021). National study on faculty and administrators’ perceptions of civility and incivility in nursing education. Nurse Educator, 46(5):276-283. https://doi: 10.1097/NNE.0000000000000948
- Forni, P. M. (2002). Choosing civility: The twenty-five rules of considerate conduct. St. Martin’s Griffin.
- Goldstein, D., Berlin, G., & Sherline, S. (2024). Revitalizing organizational health in the care delivery sector, McKinsey & Company, https://www.mckinsey.com/industries/healthcare/our-insights/revitalizing-organizational-health-in-the-care-delivery-sector
- National Academy of Medicine. (2024). National Plan for health workforce well-being. Washington, DC: The National Academies Press, https://doi.org/10.17226/26744
- National Academies of Sciences, Engineering, and Medicine. (2019). Taking action against clinician burnout: A systems approach to professional well-being. Washington, DC: The National Academies Press. https://doi.org/10.17226/25521
- Sull, D. & Sull, C. (Winter 2023). How to fix a toxic culture, MIT Sloan Management Review,
- https://sloanreview.mit.edu/article/how-to-fix-a-toxic-culture/
- Sull, D, Sull, C, Cipolli, W, & Brighenti, C. (2022). Why every leader needs to worry about toxic culture, MIT Sloan Management Review. https://sloanreview.mit.edu/article/why-every-leader-needs-to-worry-about-toxic-culture/
- U.S. Surgeon General. (2022). Addressing healthcare worker burnout: The U.S. Surgeon General’s advisory on building a thriving health workforce. U.S. Department of Health and Human Services, https://www.hhs.gov/sites/default/files/health-worker-wellbeing-advisory.pdf
- Workplace Bullying Institute. (2024). WBI definition of workplace bullying, https://workplacebullying.org/defined/
Hard Truths about the Long-Term Care Sector: Where do we go from here? - Barbara Kohnen Adriance
As a society, we have failed to provide safe, reliable, person-directed care for older adults and people living with disabilities who reside in long term care facilities. We have also failed to provide safe working environments for the hundreds of thousands of people working in these facilities. It seems that even the high-profile cases don’t generate change.
Yet all the key stakeholders – state regulatory agencies, for profit and non-profit industry associations, and the providers themselves say that they are committed to improving quality and safety. So why aren’t we seeing real change? What will it take to transform this sector?
This event will outline the key drivers of low quality and safety in long term care facilities. We will look at examples of organizations that have taken an innovative staff-centered approach to quality improvement. And we will discuss what’s next. Can we salvage the systems that we have now? Or do we need new models of care? Who needs to be at the table when new ways of care are developed? How will they be regulated? Hint: there’s a role for Oregon and Washington’s patient safety commissions.
Learning Objectives:
- Understand why long-term care facilities are not safe for residents or staff.
- Learn how some communities have made change.
- Become aware of the urgent need for change.
Resources
- LiveWell website – https://www.livewelnational.org
- Carder, P. Hasworth, S. Cater, D. (2021). Evaluation of the LiveWell Method: Final Report. PDX Scholar, Portland State University Institute on Aging.
- Institute on Aging, Portland State University, Research projects
- Kohnen, B. (2021). How LiveWell Reduces Cost and Increases Profit: Report by the Malden Collective.
- Legault, A., & Ducharme, F. (2009). Advocating for a parent with dementia in a long-term care facility: the process experienced by daughters. Journal of family nursing, 15(2), 198-219.
- Quality Measurement Program Report for Oregon Community Based Care Facilities 2023 Annual Report
Panel - Foundation for Health Care Quality, Healthcare Equity Award Winners - Kelli Houston, Nicole Jones, Van Chaudhari, Zandrea Harlin
Bree Collaborative and Foundation for Health Care Quality Award winners discuss how they create processes and practices that enhance equity that result in measurable changes in the access to and quality of care for patients.
Learning Objectives:
- Understand how collaborative care contributes to patient safety and outcomes.
- Understand how organizations embed equity principles into best practices.
- Understand specifics around quality improvement activities that are focused on equity.
Resources
Foundation for Health Care Quality
Foundation for Health Care Quality Awards
2024 Mountain Climber Award for Excellence in Health Equity Project Summaries
Bree Collaborative
Bree Collaborative Evaluation Home Page
Bree Collaborative Awards
2024 COMMUNITY HEALTH PLAN OF WASHINGTON’S Health Disparities Report
Patient decision aids to enhance shared decision making - Dan Matlock, Dawn Stacey, Randall Moseley
Patient decision aids are effective interventions for supporting patients making health and healthcare decisions. Over 200 randomized controlled trials showed compared to usual care, patients who used patient decision aids had improve decision quality, improved decision-making process, and increased participation in decision making. The International Patient Decision Aid Standards provide a set of quality criteria for defining criteria to ensure it is a patient decision aid, essential criteria for minimizing the risk of a biased decision and enhancing criteria. Current research is focused on understanding best practices for implementing patient decision aids into clinical practices and health policies.
Learning Objectives:
- Understand the state of the science supporting patient decision aids.
- Recognize challenges and facilitators for implementation of patient decision aids to enhance shared decision making.
- Learn about applications in cancer screening and cardiac treatment decisions.
Decision Aid Examples
Should I Get a Mammogram? Ages 50-74
Should I Get a Mammogram? Ages 75+
Safety, Risk, and Intersex Management - Elizabeth Reis
The term “patient safety” implies keeping patients safe from medical harm. How then might we evaluate harm that derives not from human or system error but from the medical approach itself? This presentation will explore the medical management of intersex traits (atypical sex development). Physicians have been trying to “fix” intersex since the early 19th century, and they have focused on children since the 1950s. Their efforts have been largely motivated by social anxieties about homosexuality and a sense that it would be better for children to grow up with “normal-looking” genitals, a hunch that has turned out to be wrong. Many intersex adults who have endured such “normalizing” surgeries have spoken about the physical and psychological harms that resulted from these cosmetic procedures. Though it might seem risky to let children grow up without them, activists have argued that pediatric genital surgeries violate human rights. “Patient safety” in this context would mean letting children grow up with genital, hormonal, or gonadal difference until they are old enough to make decisions about their bodies for themselves.
Learning Objectives:
- The audience will learn about the historical motivations of intersex management.
- The audience will contemplate the meaning of medical harm in the context of pediatric genital surgeries.
- The audience will expand their understanding of patient safety when considering children’s rights.
Shared Decision Making as a Strategy for Improving Patient Safety and Strengthening Relationships: One Institution’s Path to a Shared Decision Making Culture - Leigh Simmons
Dr. Simmons will share the experiences of building a culture of shared decision making at Massachusetts General Hospital, with a particular focus on programs in decision aid deployment, involvement of frontline workers in identifying areas for more shared decision making support, and supporting patients to increase their engagement with robust pre-visit preparation.
Learning Objectives:
- Identify clinical areas for shared decision making at your institution.
- Describe strategies for shared decision-making implementation.
- Examine possible barriers to SDM implementation at your institution and formulate strategies to overcome these barriers.
Systemic Racism in Health Professions Education and Possible Solutions: Enhancing Patient Quality and Safety - Daryl Traylor
This presentation addresses the issue of systemic racism in health professions education and its detrimental impact on both student experiences and patient quality and safety. Participants will gain an understanding of systemic racism, distinguish it from individual racism, and explore its historical and current manifestations within educational institutions. Through data, research findings, and real-world case studies, we will analyze the adverse effects of systemic racism on healthcare delivery, highlighting the increased risk of medical errors, health disparities, and diminished patient outcomes. The session will focus on practical solutions and strategies to mitigate these issues, including institutional changes, support systems for students, cultural competence training, and advocacy for policy reforms. Interactive elements, such as Zoom breakout discussions and case study analyses, will engage participants in reflective and solution-oriented activities.
Learning Objectives:
- Understand and Identify Systemic Racism in Health Professions Education
By the end of this session, participants will be able to define systemic racism and distinguish it from personally mediated and internalized racism, recognize its historical and current manifestations in health professions education, and understand its impact on student experiences and healthcare delivery, with a specific emphasis on patient quality and safety. - Analyze the Impact of Systemic Racism on Patient Quality and Safety
By the end of this session, participants will be able to explain how systemic racism in health professions education contributes to disparities in patient care, including increased risk of medical errors, reduced quality of care, and delayed diagnosis and treatment for marginalized groups. Participants will also engage in reflective discussions and case study analyses to identify real-world examples of these impacts. - Develop and Implement Strategies to Mitigate Systemic Racism and Improve Patient Outcomes
By the end of this session, participants will be able to propose and evaluate solutions and strategies aimed at mitigating systemic racism within their institutions. These strategies will include institutional changes, support systems for students, cultural competence training, and advocacy for policy changes, all designed to enhance patient quality and safety. Participants will also commit to actionable steps they can take in their educational or professional environments to contribute to these efforts.
The Leapfrog Group – Informing Decisions and Making Care Safe - Missy Danforth
Overview of Leapfrog’s national hospital ratings and how they can be used by patients, purchasers, and others to make hospital care safer and higher quality
Learning Objectives:
- Participants will learn about each of Leapfrog’s national ratings programs for hospitals.
- Participants will learn about which measures are included in each of Leapfrog’s programs.
- Participants will learn how patients, purchasers, hospitals, and other can use the published ratings.
Transforming BC Health Care: The Power of the Patient Voices Network - Jami Brown
The Patient Voices Network (PVN) is a community of patients, families, and caregivers who team up with health care professionals to improve health care in British Columbia. Since 2009, PVN has connected thousands of people to work together for better health care. PVN helps build strong partnerships, encourages mutual learning, and involves patients in decision-making to address health care challenges. PVN makes a difference by:
- Building Relationships
- Learning from Each Other
- Understanding Challenges and Opportunities
- Informing Decisions
Join us to hear how PVN’s collaborative approach has transformed health care in BC and learn about the exciting future of health care co-production in the province.
Learning Objectives:
- Describe at least three specific ways in which the Patient Voices Network (PVN) has connected patients, families, caregivers, and health care professionals to improve health care in British Columbia.
- Identify and explain at least two effective strategies and provide two examples of successful knowledge sharing and partnership-building between patients and health care teams, as demonstrated by the PVN, after the workshop.
- Develop a personal action plan that includes at least three specific steps to apply PVN’s collaborative principles to improve health care decision-making and practice in their own communities.
Using Physical, Testimonial and Documentary Evidence to Investigate Patient Harm Events - Jonathan Stewart
Although investigating patient harm events is an essential function of the job for many patient safety, risk management, and patient experience professionals, many find limited opportunities for training on this skill. This presentation will describe the role of investigative interviews in fact-finding, introduce the cognitive interviewing protocol, and offer practical advice for investigations in healthcare settings.
Learning Objectives:
- Describe the elements of thorough and credible investigations into patient harm events.
- Explain the Cognitive Interviewing protocol.
- Discuss the use of testimonial, documentary, and physical evidence to inform the analysis of patient harm events.
Barbara Kohnen Adriance, MPP
Hard Truths about the Long-Term Care Sector: Where do we go from here?

Barbara Kohnen Adriance, MPP
Barbara Kohnen Adriance, MPP is the Founder and CEO of The Malden Collective, a company that provides coaching and training services for teams working in long term care facilities. She is best known for creating the LiveWell Method, a quality assurance and performance improvement method that has reached more than 158 communities nationwide. Barbara has been in the health care sector 15 years, serving previously as head of training and human centered design at CareOregon, a Medicaid managed care organization. Her company has been recognized by the Oregon Department of Human Services as a contributor to improved quality of care and quality of life through its Quality Care Fund grant program. Barbara’s first career was in international policy advocacy in Washington DC, and she has deep regional experience in Central America and Mexico. Now she lives in Portland Oregon with her husband Jim and enjoys family, backpacking, and gardening with native plants.
Contact Information:
barbarak@maldencollective.com
Carolyn Canfield
A Restorative Approach to Trust and Preparing for Uncertainty

Carolyn Canfield
Carolyn Canfield works as a citizen-patient to expand partnership with patients and caregivers across all facets of healthcare: professional education, service design, practice improvement, policy development, research and governance. Widowed in 2008 by healthcare tragedy led her to full-time activism, earning recognition in 2014 as Canada’s first Patient Safety Champion. In the same year, Carolyn was appointed to faculty in the Department of Family Practice at the University of British Columbia. At UBC, she actively supports the Patient and Community Partnership for Education, the Innovation Support Unit, the Centre for Health Education Scholarship, the Gateway Clinic for interprofessional training in team-based primary care (opening 2025), patient safety curriculum and instruction, enriched learning environments, and medical school candidate selection and admissions policy for the Faculty of Medicine. Provincial, national and international healthcare research roles include patient partner, co-researcher, advisor, funding adjudicator and journal manuscript reviewer. In 2017 Carolyn co-founded the independent peer-led Patient Advisors Network patientadvisors.ca to develop citizen-patient capacity and leadership across Canada. Carolyn was a plenary speaker at the 2014 Northwest Patient Safety Conference.
Contact Information:
carolyn.canfield@ubc.ca
Cynthia Clark, Ph.D., RN, ANEF, FAAN
Civility Rising! Best Practices to Inspire Healthy Work Environments

Cynthia Clark, Ph.D., RN, ANEF, FAAN
Dr. Cynthia Clark is Founder of Civility Matters, Professor Emeritus at Boise State University and an award-winning professor, scholar, and author. As a nurse/therapist, she specialized in adolescent mental health, substance abuse recovery, and suicide and violence prevention. For two decades, Dr. Clark taught a variety of nursing courses in her role as a tenured university professor. She is a fellow in the American Academy of Nursing, the NLN Academy of Nursing Education, and co-chaired the American Nurses Association Professional Panel on Incivility, Bullying, and Workplace Violence. Her ground-breaking work on fostering civility and healthy work environments has brought national and international attention to the controversial issues of incivility in academic and work environments around the globe.
Her theory-driven interventions, empirical measurements, theoretical models, and reflective assessments provide best practices to prevent, measure, and address uncivil behavior and to create healthy workplaces. She is the recipient of numerous teaching, service, and research awards, Distinguished Visiting Scholar at 12 universities—and widely acclaimed for her engaging presentations. Her empirical assessments have been translated into 16 world languages and used by scholars in 32 countries on 5 continents.
Access to Dr. Clark’s empirical measurements, theoretical models, and reflective assessments can be obtained by browsing her Civility Matters website and scrolling to the Licensed Works link. Dr. Clark’s newest book, Core Competencies of Civility for Nursing & Healthcare is a must- read for all health care professionals which details evidence-based strategies to foster civility and healthy work environments. There is an ancillary facilitator guide and learner workbook associated with the book. The much anticipated 3rd edition of her book, Creating and Sustaining Civility in Nursing Education: A Faculty Field Guide is scheduled to be released spring 2025.
Contact Information:
cclark@boisestate.edu
Dan Matlock, MD, MPH
Patient decision aids to enhance shared decision making

Dan Matlock, MD, MPH
Dr. Matlock is Assistant Professor of Medicine, University of Colorado Health Sciences Center. He is a clinician-researcher with a strong interest in medical decision making and patient-centered care. Specifically, focusing on how older and sicker adults make decisions about invasive technologies using implantable defibrillators as a model.
Contact Information:
daniel.matlock@cuanschutz.edu
Danielle Ofri, MD, Ph.D., D.Litt (Hon), FACP
Opening Keynote – When We Do Harm: Medical Error and the Human Condition

Danielle Ofri, MD, Ph.D., D.Litt (Hon), FACP
Danielle Ofri, MD, PhD is a primary care internist at Bellevue Hospital, the oldest public hospital in the country. She is Founder/Editor-in-Chief of the Bellevue Literary Review, and is a clinical professor of medicine at NYU School of Medicine.
Danielle Ofri is the author of six books about life in medicine:
- When We Do Harm: A Doctor Confronts Medical Error
- What Doctors Feel: How Emotions Affect the Practice of Medicine
- Medicine in Translation
- What Patients Say; What Doctors Hear
- Incidental Findings
- Singular Intimacies: Becoming a Doctor at Bellevue
Danielle Ofri writes about medicine and the doctor-patient relationship for the New Yorker, the New York Times, the Lancet, and the New England Journal of Medicine. Her articles have also appeared in Slate Magazine, the Los Angeles Times, the Washington Post, the Atlantic, CNN and on National Public Radio.
She was also editor of a medical textbook—The Bellevue Guide to Outpatient Medicine—which won a Best Medical Textbook award.
Her writings have been selected twice for Best American Essays and also for Best American Science Writing. She has received the McGovern Award from the American Medical Writers Association for “preeminent contributions to medical communication,” and an honorary doctorate of humane letters.
Other recent awards include:
- 2023 Guggenheim Fellowship
- 2023 Davies Memorial Award from the American College of Physicians
- 2022 National Humanism in Medicine Medal from the Gold Foundation
- 2020 Global Listening Legend Award
Danielle Ofri has given TED talks on Deconstructing Perfection and Fear: A Necessary Emotion, and has also performed stories for the Moth. She is featured in the documentaries “Why Doctors Write” and “White Coat Rebels.”
An ever-struggling student of the cello, she is slogging—ever so slowly—through all 36 movements of the Bach cello suites.
Daryl Traylor, M.S., MPH, Ph.D.
Systemic Racism in Health Professions Education and Possible Solutions: Enhancing Patient Quality and Safety

Daryl Traylor, M.S., MPH, Ph.D.
Daryl Traylor is an academic and researcher, currently serving as a faculty member at Eastern Washington University. With a background in teaching and research, he has worked in T-cell and HIV biology, HIV PrEP, and cancer biology. Daryl’s educational journey reflects his dedication to learning and the sciences, holding multiple advanced degrees and currently expanding his knowledge as a medical student, MBA-Healthcare Administration student, and DrPH student. Originally from Houston, Texas, he lived in Chandler, AZ for 16 years, following a 20-year service in the Active Duty Army, Oklahoma Army National Guard, and Oklahoma Air National Guard. Daryl now resides in San Antonio, Texas with his wife Eboni and their two cats, Loki and Thor.
Contact Information:
dtraylor1@ewu.edu
David Newman-Toker, MD, Ph.D.
AI for Clinical Diagnosis at the Crossroads: A Tale of Two Possible Futures

David Newman-Toker, MD, Ph.D.
David Newman-Toker, M.D. Ph.D. is Professor of Neurology, Ophthalmology, and Otolaryngology, and is the inaugural recipient of the David Robinson Professor in Vestibular Neurology. He holds joint appointments in Emergency Medicine and Health Sciences Informatics at the Johns Hopkins University School of Medicine, as well as in Epidemiology and Health Policy & Management at the Johns Hopkins Bloomberg School of Public Health.
Dr. Newman-Toker’s academic mission is to eliminate harms from diagnostic errors and maximize the accuracy and efficiency of diagnostic testing in clinical practice. He is as a Core Faculty member of the Armstrong Institute for Patient Safety & Quality, where he serves as Director of the Armstrong Institute Center for Diagnostic Excellence, focused on enhancing diagnostic safety, quality, and value.
Dr. Newman-Toker’s research focuses on preventing missed strokes in the emergency department and primary care, especially among patients presenting with acute, severe vertigo or dizziness. He and his collaborators have developed innovative methods to diagnose stroke through careful bedside examination of eye movements. He is now translating these innovations into clinical practice through the use of novel technologies at the point of care.
Dr. Newman-Toker’s clinical expertise is in disorders of the brainstem and cranial nerves, including visual loss, double vision, and vertigo. He serves as Director of the Division of Neuro-Visual & Vestibular Disorders. His clinical practice focuses on emergency evaluation of patients with acute vertigo and dizziness. He does not currently have an outpatient clinic practice.
Dr. Newman-Toker completed his undergraduate education at Yale University (B.S., 1991) and his medical training at the University of Pennsylvania School of Medicine (M.D., 1995). After completing his Neurology residency at the Massachusetts General Hospital (1999), he went on to complete fellowships in Neuro-Ophthalmology at Harvard University/Massachusetts Eye & Ear Infirmary (2000) and in Neuro-Otology at the Johns Hopkins University School of Medicine (2002). He completed his doctoral training in clinical research methods at the Johns Hopkins Bloomberg School of Public Health through the Graduate Training Program in Clinical Investigation (Ph.D., 2007).
Contact Information:
toker@jhu.edu
Dawn Stacey, RN, PhD, FRSC, FCAHS, FAAN, FCAN
Patient decision aids to enhance shared decision making

Dawn Stacey, RN, PhD, FRSC, FCAHS, FAAN, FCAN
Dawn Stacey is the Vice Dean Research in the Faculty of Health Sciences of University of Ottawa, Canada. She holds a Research Chair in Knowledge Translation to Patients and is the Co-Scientific Director of the Patient Decision Aids Research Group at the Ottawa Hospital Research Institute. Her research uses co-production to develop, evaluate, and implement interventions to support patients and their families to be involved in healthcare decisions. With her outstanding and continuous accomplishments in research, she has received fellowships with the Royal Society of Canada (FRSC), American Academy of Nursing (FAAN), Canadian Academy of Health Sciences (FCAHS), and the Canadian Academy of Nursing (FCAN).
Contact Information:
dstacey@uottawa.ca
Elizabeth Reis, Ph.D.
Safety, Risk, and Intersex Management

Elizabeth Reis, Ph.D.
Is a professor at the Macaulay Honors College at the City University of New York where she teaches courses on Medical Ethics; Reproductive Technologies; Gender, Sex, and Bioethics; and Disability Studies. She graduated from Smith College and received her Ph.D. in History at the University of California, Berkeley. Reis is the author of Bodies in Doubt: An American History of Intersex (2nd edition 2021); Damned Women: Sinners and Witches in Puritan New England; and the editor of American Sexual Histories. She has published essays in the Hastings Center Report, Bioethics Forum, Journal of American History, Perspectives in Biology and Medicine, the New York Times, and TIME Magazine. Reis is a member of the Ethics Committee at New York Presbyterian Weill Cornell Hospital and an editor of Nursing Clio, a collaborative online journal that focuses on the intersection of gender, history, and medicine. She is a former board member of interACT: Advocates for Intersex Youth and a current board member of Talia’s Voice: Projects for Patient Safety.
Living an intersex life, CBS Sunday Morning
Contact Information:
elizabeth.reis@mhc.cuny.edu
Health Equity Award Winners - - Kelli Houston, Leo Sergio Morales, MD, Nicole Jones, Natalia Usoltseva MD, FACP, MHAi, Zandrea Harlin
Foundation for Health Care Quality, Award Winners Round Table
Kelli Houston
Kelli Houston is the Chief Equity Officer for Community Health Plan of Washington (local not-for-profit, serving vulnerable members throughout the state of Washington), where she is responsible for leading DEI strategic planning and execution across the organization. She is the chair of the statewide Equity Council and serves on several community-led committees overseeing key priorities in advancing organizations with an anti-racism approach. She comes to us with over 17 years of DEI Leadership experience across the health and human sector with emphasis on health and racial equity and ensuring that culturally diverse communities live healthier lives and receive the care they need and deserve.
Contact Information:
kelli.houston@chpw.org

Leo Sergio Morales, MD
Leo Sergio Morales, MD, is a Professor and Assistant Dean with the Office for Health Care Equity at UW Medicine. He also serves as co-director for the Latino Center for Health, a state funded interdisciplinary health sciences research center focusing on Latino health issues in Washington State and the Pacific Northwest region. Dr. Morales received his medical degree and Master’s degree in public health from the University of Washington, and his doctorate in policy analysis from the Rand Graduate School. He completed an internship and residency in primary care internal medicine at the San Francisco General Hospital/UCSF and a fellowship in primary care research at UCLA. Prior to joining the faculty at the University of Washington in 2014, he was a faculty member at UCSF and UCLA schools of medicine and an investigator at the Group Health Research Institute.
Contact Information:
lsm2010@uw.edu

Natalia Usoltseva MD, FACP, MHA
Natalia Usoltseva MD, FACP, MHA is an internal medicine physician, practicing as a PCP for the last 10 years who received a master’s degree in Health Administration at the University of Washington. Over the past 5 years, she has been serving as a clinical medical director to support operations and provide on-site leadership at primary care and urgent care facilities. She has also served as a physician lead for the population health at UW Primary Care and chair of the UW Medicine Population Health Committee for Equity and Quality of Adult Ambulatory Diabetes Care.
Contact Information:
usoltsev@uw.edu

Nicole Jones
When not enjoying the scenic hiking trails of Washington, Nicole Jones works for UnitedHealthcare Washington State Medicaid plan as the Behavioral Health Clinical Director. Nicole is a licensed clinical social worker and certified substance use disorder professional, who has obtained additional mental health specialties for working with children and geriatric populations, as well as individuals with intellectual disabilities. Nicole holds a master’s in business administration with concentrations in finance, general business, international business, and accounting. Her varied career within the Medicaid marketplace, working in residential treatment, crisis services, utilization management, and clinical administration, has fueled Nicole’s passion for finding innovative products to improve service and care for the members she serves.
Contact Information:
nicole.jones1@uhc.com

Zandrea Harlin
Zandrea’s clinical nursing background is in behavioral health. She started her career in community mental health and spent the thirteen years working at Kaiser Permanente Washington. Zandrea is passionate about using her frontline clinical perspective and public health skills to help build care delivery systems that deliver on the promise of equity, quality, service, and cost.
Zandrea also worked as a primary care leader and for the last 10 years she has worked in a variety of roles in Quality and Population Health. Zandrea is currently the Director of Quality at Kaiser Permanente Washington and loves to explore the structural and programmatic ways to improve the health of our members and communities. Zandrea is honored to support teams with accreditation, safety, quality improvement, and reporting, and her favorite part of her role in quality is partnering with teams and patients to identify health disparities and develop strategies to eliminate them.
Contact Information:
zandrea.t.harlin@kp.org
Jami Brown, Annmarie Elderkin, Hugh Alley
Transforming BC Health Care: The Power of the Patient Voices Network

Jami Brown
Engagement Leader, Patient & Public Engagement. Jami joined Health Quality BC in February 2016, where she brings her passion for working with people to her role as an Engagement Leader. Prior to joining the Council, she led the communications and engagement strategy for the largest provider of seniors housing in British Columbia. Before that, she spent 10 years at Fraser Health leading a multidisciplinary team focused on creating healthier communities. Throughout her career, Jami has enthusiastically supported doing everything she can to draw on the richness of our collective experiences to build a health care system that works for everyone. Jami holds a Master of Arts in Professional Communication from Royal Roads University, a Bachelor of Arts in Communications from Western Washington University and is a certified trainer in Public Participation and LEAN Healthcare.
Contact Information:
jami.brown@healthqualitybc.ca

Annmarie Elderkin – Patient Partner, Vancouver Island, British Columbia
I am a Patient Advisor and a survivor of childhood sexual abuse, severe bullying from kindergarten through high school, physical and emotional abuse by a sibling, emotional abuse from my war veteran father, and severe emotional and physical abuse from my spouse.
As an adult, I began my recovery journey with “Here and Now Therapy.” This approach allowed me to talk about my past for only five minutes. Instead, I focused on my plans for today, tomorrow, next week, next month, the next six months, and the upcoming year. During this time, I was diagnosed with severe depression, bipolar disorder, schizophrenia, psychosis, and post-traumatic stress disorder (PTSD). I refer to my voices as “the Background Interference Committee.” I am pleased to share that after more than 20 years of trying various medications, I have found success with Abilify by injection. This medication, combined with a healthier diet that includes fewer carbs and sugars, has given me a new lease on life. Additionally, the symptoms of my conditions were exacerbated by untreated diabetes in my earlier years.
I also run Annmarie’s Angel Network, where I source resources and services for low-income seniors and individuals with disabilities. I request items online, and wonderful people across Canada and the USA generously donate what is needed. My clients and I are truly grateful for their kindness.
I became a Patient Advisor several years ago with the Patient Voice Network on a COVID-19 committee. I later joined the Red Fish Healing Centre and Heartwood as a Patient Advisor. Through my experiences with these committees, I successfully contributed to the Enhanced Crisis Line Committee, where I hope to leave a legacy of positive change. I strive to be a voice for those who feel unheard in these committees and focus groups.
My dream job is to gain the skills and abilities necessary to work full-time as a peer support worker in a psychiatry unit once I improve my physical health. I take pride in my part-time role as a Community Support Worker for the Nanaimo Community Living Association (NACL) and my volunteer work with the Patient Voice Network (PVN). I encourage others to become Patient Advisors as well.
On my Journey I wrote three books and published two on Amazon. My Children did suffer because of my returning to Halifax from Yellowknife however both in their Adult lives received counselling and are thriving. One is pursuing their master’s degree in education and the other has opened an Ayawaska, Psychedelic Treatment Residence on Vancouver Island.
I want to express my heartfelt gratitude to all the wonderful caregivers who have made a remarkable difference in my life and the lives of my family, community, nation, and world. I especially appreciate the care and patience of my children, family, and extended family.
I have been under the care of cardiologists since birth. For the last 30 years, I’ve been monitored at the Pacific Adult Congenital Heart Clinic at St. Paul’s Hospital. During one of my regular checkups, I noticed a bulletin seeking Patient Partners. Since 2019, I have been an active Patient Partner, participating in over 15 different engagements.

Hugh Alley – Patient Partner, Metro Vancouver, British Columbia
I am a husband, father, author, consultant, and much more. Personally, I’ve been married to my amazing partner for over 30 years, and we have two adult children who have successfully launched into their own lives. We’re especially excited that our son just got married!
Professionally, I have primarily worked as an industrial engineer, managing three factories and a department within a government agency. I’ve written two books focused on developing front-line supervisors, and I frequently appear on podcasts, regularly writing and speaking about front-line leadership and continuous improvement. My hope is that my efforts help create better work environments for others.
I am also a patient, though that does not define me. I was born with a complex set of congenital heart defects and spent a significant amount of time in hospitals as a child. These experiences have shaped my outlook in ways I am still discovering. The open-heart surgery I underwent at the age of two was developed just six months prior, and a second surgery at seventeen replaced a failed valve.
As an adult, I have remained active, enjoying skiing, sailing, cycling (including extended road trips), canoeing, and kayaking. In my early forties, I received my first pacemaker, and I am now on my fifth device—an implantable defibrillator—and I am 100% paced. I continue to stay active through hiking and kayaking. In 2010, I competed at the National Masters Regatta, and in 2019, I enjoyed a week-long kayaking trip in Haida Gwaii. Most people who meet me have no idea about my medical history, and I prefer it that way.
I have been under the care of cardiologists since birth. For the last 30 years, I’ve been monitored at the Pacific Adult Congenital Heart Clinic at St. Paul’s Hospital. During one of my regular checkups, I noticed a bulletin seeking Patient Partners. Since 2019, I have been an active Patient Partner, participating in over 15 different engagements.
Jonathan Stewart, JD, MSc, MS, RN, CPPS, CPHRM
Using Physical, Testimonial and Documentary Evidence to Investigate Patient Harm Events

Jonathan D. Stewart, JD, MSc, MS, RN, CPPS, CPHRM
Jonathan D. Stewart, JD, MSc, MS, RN, CPPS, CPHRM is a patient safety professional, healthcare risk manager, and educator. He oversees the provision of BETA Healthcare Group’s consultation, education, and risk assessment services to hospitals, healthcare facilities, and medical groups. Prior to joining BETA, Mr. Stewart served as the Patient Safety Officer for the Veterans Health Administration’s Northwest Network (VISN20). He is experienced in both administrative and adverse event investigations, and in facilitating root cause analyses. He is a past chair of the Washington Patient Safety Coalition steering committee and is a past president of the American Association of Nurse Attorneys. Mr. Stewart received his law degree from the University of Tulsa and holds master’s degrees in nursing/health policy from the University of California at San Francisco and in human factors and system safety from Lund University in Sweden.
Contact Information:
jonathan.stewart@betahg.com
Leigh Simmons, MD
Shared Decision Making as a Strategy for Improving Patient Safety and Strengthening Relationships: One Institution’s Path to a Shared Decision Making Culture
Leigh Simmons, MD, is an internal medicine physician at Massachusetts General Hospital and assistant professor of medicine at Harvard Medical School.
She is the Medical Director of the MGH Health Decision Sciences Center where she studies the use of decision aids to help patients and clinicians in the shared decision making process. Dr. Simmons develops and conducts training of physicians and staff in communication skills focused on improving decision making with patients. Her clinical practice is with the Internal Medicine Associates at Massachusetts General Hospital. In addition to her clinical and research interests, Dr. Simmons is a medical student educator and directs the internal medicine clerkship for Harvard Medical School students at Massachusetts General Hospital.
Contact Information:
lhsimmons@mgh.harvard.edu
Missy Danforth
The Leapfrog Group – Informing Decisions and Making Care Safe

Missy Danforth
Missy Danforth is the Senior Vice President of Health Care Ratings at The Leapfrog Group, a Washington, DC based, not-for-profit organization representing the nation’s largest employers and purchasers of health benefits working to make great leaps forward in the safety, quality, and value of healthcare.
At Leapfrog, Ms. Danforth serves as member of Leapfrog’s senior leadership team informing Leapfrog’s strategic direction, engaging experts and stakeholders, and analyzing program results to engage purchasers and consumers and to drive safety and quality improvements. Ms. Danforth administers Leapfrog’s various measurement and public reporting activities including the Leapfrog Hospital and Ambulatory Surgery Center Surveys, the Hospital Safety Grade, Leapfrog’s Value-Based Purchasing Program, the Leapfrog’s new recognition program, which recognizes hospitals providing exceptional care for patients with diabetes, in partnership with the American Diabetes Association.
Ms. Danforth services on the governance board of Battelle’s Partnership for Quality Measurement (PQM), is the former chair of the National Quality Forum’s Consensus Standards Approval Committee (CSAC) and serves on various other national committees and technical expert panels. She is currently leading a four-year project to develop national standards for diagnostic safety and quality in hospitals.
Contact Information:
mdanforth@leapfrog-group.org
Randy Moseley, MD
Patient decision aids to enhance shared decision making
Randy Moseley, MD
Dr. Moseley received his M.D. from the University of Washington. After completing an Internal Medicine residency at the University of Utah, he practiced General Internal Medicine in rural Wyoming for 15 years before returning to Washington State and joining Wenatchee Valley Medical Center (now Confluence Health). He founded their Hospitalist Service in 2002, and with this began to realize the importance of systems of care in the quest to improve care quality and outcomes. This led to a career transition into health care quality beginning in 2007. He recently retired from his position as Medical Director of Patient Safety and Risk at Confluence Health. His quality improvement work included enhancing care quality through structured team communication, fostering an organizational culture of safety, promotion of shared decision making and patient engagement, and optimizing the approach to medical errors. His engagement on the state level has included work with the Washington Patient Safety Coalition, the Washington Health Alliance, the Washington State Choosing Wisely Taskforce, the Washington State Hospital Association Patient Safety Committee, the Robert Bree Collaborative, and Communication and Resolution Program adoption.
Contact Information:
Randal.Moseley@confluencehealth.org
Sian Hsiang-Te Tsuei, MD, Ph.D.
Artificial Intelligence and health care: Its applications and hidden dangers
Sian Hsiang-Te Tsuei, MD, Ph.D.
Dr. Sian Tsuei (Shawn Tsu-ay) MHSc, MD, PhD, CCFP is a practicing Canadian family physician with Population Health Sciences PhD from Harvard University. He is a Clinical Assistant Professor (UBC), Adjunct Professor (SFU) and Visiting Scientist (Harvard University). He is currently a member on the Artificial Intelligence Advisory Group of the College of Family Physician of Canada. His research examines health systems change related to technologies. He is particularly interested in the how AI affects the behaviours of health care providers and patient, as well as how AI affects the provider-patient dynamics. His research is global in nature, and he has particular interest in the Asian and North American contexts.
Contact Information:
sian.tsuei@gmail.com
We are pleased to invite interested sponsors to support our 21st annual conference. As a sponsor you are helping to subsidize the cost of the conference to healthcare staff and provide free attendance to patients, families, and students.
THIS YEAR’S PACKAGES OFFER SEVERAL LEVELS FROM WHICH TO CHOOSE.
Details of package benefits are described in the application.
- Platinum Sponsor – $10,000 (1 available)

- Gold Sponsor(s) – $7,500 (3 available)
- Silver Sponsor(s) – $5,000
- Bronze Sponsor(s) – $2,500
- Supporter(s) of Patient Safety – $1,500
All sponsors will be recognized on the Washington Patient Safety Coalition website and marketing materials with sponsor logos linking to a webpage of your choice.
Platinum, Gold, Silver and Bronze sponsors have access to a dedicated page on the conference website which can include images, videos, links, etc.
WELCOME TO THE 2024 21st ANNUAL NORTHWEST PATIENT SAFETY CONFERENCE!
For those who were able to attend the live conference, we hope you enjoyed it and learned plenty!
If you were not able to attend the live conference, do not worry, we will be uploading the conference sessions in the event portal on November 4. To gain access to the portal and watch the sessions, you will be required to enter your attendee confirmation code. You can find your code at the very bottom of your registration confirmation email or by clicking HERE and entering your email to get it resent. If you continue to have trouble getting in, please contact Steve Levy at 206-204-7383 or Amelina Kassa at 206-204-8384.
HOW TO APPLY FOR CE CREDITS FOR THE LIVE CONFERENCE PRESENTATIONS:
All conference registrants should have received an email with subject “SURVEY/C.E. APPLICATION: 2024 NW Patient Safety Conference” sent by email wpsc@qualityhealth.org. If you were registered and did not receive the survey email, please contact Amelina Kassa at akassa@qualityhealth.org so you can get the link emailed to you and take the survey. For CE credits go directly to question 12. However, we encourage you to complete the entire survey and provide us with feedback! Upon receipt of your survey/CE application, we will either send you a certificate(s) or for CNEs we will send you a required questionnaire about each presentation.
RECORDED PRESENTATIONS:
The conference presentations will be posted on the conference event portal on November 4. To view the recorded presentations, log into the event portal at the “enter event portal here” button above and enter your attendee confirmation code (you can find your attendee confirmation code at the very bottom of your registration confirmation email or by clicking HERE and entering your email to get it resent.) Once you are logged into the portal, click on the “Info” tab at the top of the page. The presentations, slides, and supporting materials will all be posted here sorted by presentation date and time.
HOW TO APPLY FOR CE CREDITS IF YOU VIEW THE RECORDED PRESENTATIONS:
In the event portal, toward the top of the “Info” page is a section called “How to get educational credits.” In this section is a link to a CE application form used for the recordings. Use this for all recorded presentations. Upon receipt of your CE application, we will send you the certificate(s).

ART SPEAKS
For the second year, WPSC’s Addressing Stigma & Bias Workgroup is featuring artwork as a powerful way to connect with patients’ experiences with health conditions. Our focus this year is mental illness & behavioral health.
Art is not only beautiful, it is a potent medium of expression. Evocative and compelling, it touches the soul and connects in a way no other medium can.
Featured artwork this year include art and a poem by PNW residents Louie Gong, Mahvish Naqvi, Munira Leslie Sinclair and Anita Sulaiman as well as a poem by model-turned actress and mental health advocate, Cara Delevingne. Big thank you to the artists for sharing their compelling pieces with us.
**************************************************************************************************************************************************************************
Visual Art
**************************************************************************************************************************************************************************

ART PIECE: Black Sheep
Click here for a video showing the making of this piece
ARTIST NAME: Louie Gong
Click here for artist’s biography and link to Eighth Generation.
ARTIST INFO: Louie Gong (Nooksack) is the founder of Eighth Generation. A self-taught artist who was raised by his grandparents in the Nooksack tribal community in northwest Washington, he got his start by painting cultural art on shoes.
Realizing that creating one-of-a-kind pieces did not provide a sustainable pathway to success, he began applying his artwork to accessibly priced products. His unique style merges traditional Coast Salish art with influences from his mixed heritage and urban environment to create work that resonates widely across communities and cultures.
Black Sheep is about drawing power from past experiences— even traumas. It is about self-care.
“I’ve been thinking about the term baggage, and it’s all wrong. When we think about our past experiences as something we can just put down, we can’t actually heal. The real pathway to becoming stronger and more confident versions of ourselves is to learn to live in symbiosis with our past experiences.”
The Black Sheep’s body is composed of Louie’s signature wolf-mouth motif, which he uses here to symbolize negative past experiences. It is painted loosely to indicate the frequent movement of and the idea that our past experiences are living parts of us that we can’t simply set down as if they were “baggage.”
By contrast, the Black Sheep’s face is composed of highly structured Coast Salish design elements to indicate the self-confidence drawn from the understanding that past experiences make us better equipped to manage whatever lies ahead. A few understated sprouts indicate constant growth regardless of what we are experiencing.
__________________________________________________________________________________________________________________
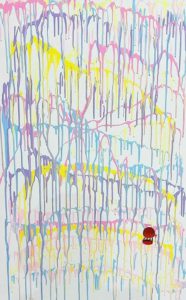
ART PIECE: Bleed Joy
ARTIST NAME: Tahira Naqvi
ARTIST INFO: I am a new artist venturing out to create artwork that speaks to mental health struggles. Childhood trauma is a big factor in my art, which is abstract and comes from the heart. It delves into deep wounds and the quest to achieve joy through self-reflection. I speak through colors and shapes that represent this journey of self-healing.
When I started on this piece, I did not know what to create, but I knew I wanted to display my pain, my joy, and my journey. So, I faced the canvas and decided to just let it flow. This piece has chaos, joy and a dark passenger. All representing the struggle between my child and adult selves. There is a hot air balloon. When I was little, I always wanted to escape. One day, I took my mom’s large shoe box and tied her red scarf to its four ends, after which, I walked out to our balcony and tried to leap off to go explore the world. Except, my grandfather saved me.
I have a natural instinct to leap forward and escape. It took cycles of anxiety to create this very personal piece. “Bleed Joy” is for everyone dealing with mental chaos and anxiety in their lives. My hope is that, by putting this out there, I will finally heal and find contentment.
_________________________________________________________________________________________________________________
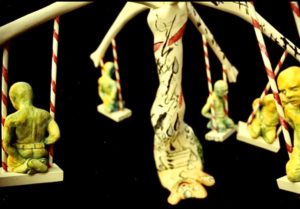
ART PIECE: Untitled
ARTIST NAME: Munira Leslie Sinclair
ARTIST INFO: Munira Leslie Sinclair was a talented visual artist, eloquent writer & devoted mother to her children, including an adult son with severe traumatic brain injury (TBI). Much of her artwork was inspired by her struggles through some very difficult times as well as the unrelenting challenges of trying to ensure quality care for her son with special needs, in a system not well set up for patients like him. A passionate patient advocate, she worked to improve the lives of those with TBI through legislation & advocacy training. While she faced adversity & bouts of cancer with fortitude, art was her outlet.
Leslie passed away on September 30, 2022. Special thanks go to her daughter, Jennifer, who has given WPSC’s Addressing Stigma & Bias Workgroup permission to share these 2 pieces with our audience.
_______________________________________________________________________________________________________________
ART PIECE: Safe Space
ART PIECE: Trapped

ART PIECE: Underwater
ARTIST NAME: Kaycia Ogata
Click here for artist’s biography and link to Eighth Generation.
ARTIST INFO: Kaycia Ogata is a graphic designer and illustrator, living and working in Portland, Oregon. Art has always been a form of therapy for her, as she lived with some depression and anxiety from a young age. Not being able to form the words she needed, she drew them. Underwater was created in remembrance of her mother’s passing when she was a child, and that sense of wanting to retreat deep into the ocean. Safe Space and Trapped were both created at the start of the pandemic, when the entire world locked down, capturing that sense of fear, isolation and uncertainty. More of her work – including design – can be found on her website
_________________________________________________________________________________________________________________
ART PIECE: Freed: Dawning, Lightened, Lifted
ART PIECE: Bangau
ARTIST NAME: Baacooly
ARTIST INFO: Baacooly is a self-taught artist hailing from a small town in culturally rich Penang, Malaysia. She creates her art pieces in watercolour with a little mixed media thrown in. Female characters are her preferred subject matters, painted in the surreal style. They are often portrayed as seemingly lost in thought. She draws inspiration from her own experiences in life and whatever is tugging at her heart the most when she is working on her creations. Rather than explain her thoughts behind each piece, Baacooly prefers for her audience to draw their own conclusions & conjure their own stories when they view her paintings. More of her work can be found on her website
_________________________________________________________________________________________________________________
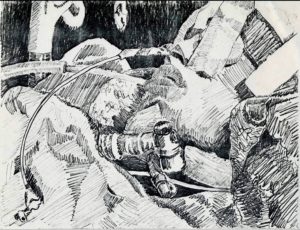
ART PIECE: There Is No Patient Safety
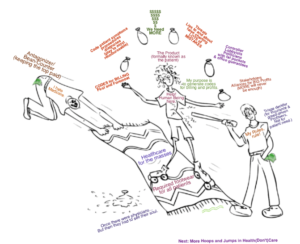
ART PIECE: Wound? I Don’t See A Wound.
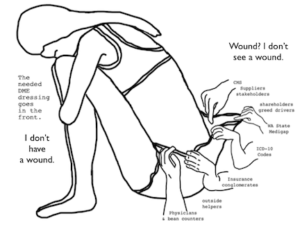
I’ve been fighting for my DMEs to be reinstated for six years now. Anyway, that’s what this drawing is about. I just shake my head at the stupidity of those in charge, making major medical decisions on peoples lives — like I said, if they had a brain, they’d seriously take it out and play with it. And the biggest crime of all, is all forgot to include the patient, or to remember that there’s actual human life involved.
ARTIST NAME: Marcía A.
ARTIST INFO: I am an artist, photographer, illustrator, and have 3 published children’s books. I’ve been a photographer for most of my life and a mixed media artist. I had my own studio/gallery for quite some time. The satirical write ups and sketches have been an outlet – especially through the frustrating nightmare of Health (don’t) Care in America, and most definitely in Washington state, and the stupid screwup with my DME six years ago. I think the sketches keep me from cussing a blue streak, which I’ve also done out of necessity. The Joint Commission and those that taught me how to be a proactive patient back in the 1980s, told me to speak up. They said if I’m not being heard or they’re not listening, to speak louder or shout, and if they’re still not listening — cuss a blue streak until you get their attention because it’s about your health and your life.
The purpose of life, is the life of purpose.
Practice random acts of kindness.
**************************************************************************************************************************************************************************
Poetry
**************************************************************************************************************************************************************************
EVERYTHING CHANGES
Everything is touched
by the sea of time.
We are life forms
on the shore
of existence.
No matter how you try
to be immovable,
time moves you.
It caresses you,
lulls you,
embraces you.
Just as you’re buoyed
into a comfortable slumber,
it snatches you,
pulls you out
& swallows you.
It swirls you around
& sucks you in.
Then,
just as suddenly,
it floats you,
breathless,
onto its surface.
The winds of change
calm to a whisper.
You feel it
cushioning you,
as you lay
adrift
with your face to the sky.
Then it stirs,
picks you up,
carries you
on a wave;
pushes you forward,
races you
back to shore
& deposits you,
gently,
onto the sand.
Glistening in the sun,
you catch your ragged breath. And settle down.
Before long,
you’re feeling the breeze
on your face,
looking up at the stars
& thinking:
I could stay like this forever.
You inhale the stillness…
Then it wakes you
from your reverie.
It foams
at your feet,
kissing your toes,
nudging you.
It teases you
into motion.
Slowly,
you move to the tide’s rhythmic touch,
sway to its hypnotic gyrations
& join,
again,
the dance of life.
—
Tomorrow becomes today.
Today becomes yesterday. Yesterday is but a memory.
Did we remember to live in today?
© 2020 Anita Sulaiman
POEM TITLE: EVERTHING CHANGES
ARTIST NAME: Anita Sulaiman
ARTIST INFO: Anita Sulaiman is Principal Consultant and Executive Coach at IBEX Consulting, whose areas of expertise include strategy, leadership development, marketing and change management/business process re-engineering. Anita is also a culture coach specializing in cultural competency and cross-cultural communication. Helping individuals and organizations excel in a global world is a passion.
Anita stays at the forefront of efforts to improve patient safety, serving on advisory groups and committees for organizations including the Washington Patient Safety Coalition, Foundation for Health Care Quality (Patient & Family Advisory Council) and Washington State Coalition for Language Access. She is Chair of the Addressing Stigma and Bias Workgroup, a partnership between WPSC and the Bree Collaborative, a healthcare non-profit established by the Washington State Legislature.
Everything Changes was written at a time of emotional turmoil. In the midst of personal upheaval, thanks to the practice of meditation to help with her mental health, this poem about the vagaries of time captures moments of clarity from seeing that change, while invariably very stress-inducing, are part of the ebb & flow of life.
_________________________________________________________________________________________________________________
MOTHER
Mother
You are & you aren’t her
You’ve had to be mother & father
Did you know – you were the world to me?
Your eyes the window through which I see
Mother
Not a word to use in vain
So why are you my biggest source of pain?
You are the reason I am here
You are the idea I hold dear
What is this figure?
We call mother
What is this idea?
No other thing comes near
She is a hug
A warm embrace
Someone who’s there to kiss your face
To hold your hand
To wipe your tears
She’s there to chase away your fears
She is the reason
You stand strong
Can tell the difference between right & wrong
She is your shelter
From the storm
The well you get your reassurance from
At least that’s what
Everyone seems to think
They don’t know yours pushed you to the brink
Put you down
And cast you out
Always wished she could’ve done without
Mine gave me a bit of love
And a lot of hate
Served honey & poison on the same plate
Was never there
To kiss my face
But she made sure I always knew my place
I had no shelter
From storms or even rain
What I had
Would drive most people insane
There was no one
To wipe away my tears
I had someone filling my heart with fears
While you had hugs
Someone to hold your hand
I had to figure out where I stand
You always knew
Where you belong
All I was ever told was I was wrong
Wrong to want
To ask or to question
To live for others – that is my mission
You had wind beneath your wings?
Me?
Who am I to have needs or feelings?
While you had kisses
A friend & all
Someone to catch you when you fall
I had no right
To be happy
Yes, that was what she said to me
So don’t tell me
How I’m supposed to feel
You don’t know what for me is real
Don’t bother
To pile on the guilt
That’s the foundation on which I was built
All that said
Good comes with bad
She’s the only mother I’ve ever had
The person
Who instilled in me
All the good things that to this day you see
She taught me
Through trial by fire
How to prevail & always aim higher
Yes, I suffered
A million cuts
I also have the biggest heart of hearts
Mummy
If you only knew
All the love I have in my heart for you
To me
You gave birth
Yet for some reason
You don’t know my worth
I am
Pure love
A blessing
A gift from the Lord above
That is what babies are
Not a thing comes close
Not even by far
Today
I make peace
With all that was, will be & all that is
I can’t forget
But I forgive
You were only doing your best to live
In return
These things I ask
No more pretenses
Take off your mask
It’s time
Let go
Set yourself free
From who you think you’re supposed to be
I am trying
To do the same
Life is too short
For anger or for blame
I hope you see
That just like you
I am human
I’m doing my best too
All my life
Through all the hurts
I’ve been held to impossible standards
Now I know
It’s clear to me
Those high bars
Were what you were made to see
On this day
I hereby purge
I release
So we both can finally have peace
From here on
May we know
Acceptance
And a better tomorrow
Happy Mother’s Day.
© Anita Sulaiman 2023
POEM TITLE: MOTHER
ARTIST NAME: Anita Sulaiman
ARTIST INFO: Anita Sulaiman is Principal Consultant and Executive Coach at IBEX Consulting, whose areas of expertise include strategy, leadership development, marketing and change management/business process re-engineering. Anita is also a culture coach specializing in cultural competency and cross-cultural communication. Helping individuals and organizations excel in a global world is a passion.
Anita stays at the forefront of efforts to improve patient safety, serving on advisory groups and committees for organizations including the Washington Patient Safety Coalition, Foundation for Health Care Quality (Patient & Family Advisory Council) and Washington State Coalition for Language Access. She is Chair of the Addressing Stigma and Bias Workgroup, a partnership between WPSC and the Bree Collaborative, a healthcare non-profit established by the Washington State Legislature.
Mother’s Day is a tough one for me. This year, I struggled as I did in previous years. Except, this year, my mother, who recently turned 80, is very ill. Her condition has intensified for me all the emotions tied to her. This poem is dedicated to all who can relate.
Usually, the words just come. I have to scribble quickly & I am done. This time, I struggled. The words wanted to come out, but… Something in me resisted. I had to fight to let these truths out. To give them the light of day felt like giving my pain validity.
Writing down these words meant staring my trauma in the face. It meant ripping off the plaster. In the end, it was exactly what needed to be done. This is validation I needed to gift to myself. I am giving myself long overdue permission to feel, to acknowledge. It is what it is. No matter what people say, it’s ok. It’s not right, but it’s ok. With that realization comes release.
My poems are medicine to me. Sometimes they are light that shows the way – guidance from a place of pure love. Now I can start to heal, God willing.
This is my art; my outlet; expression from the deeper parts of me. This is my balm; my inspired remedy. This is healing for my soul. Poetry, for me, is all that & more. It’s my connection with the Divine. It is divine.
WHO AM I TRYING TO BE?
Who am I? Who am I trying to be?
Not myself, anyone but myself.
Living in a fantasy to bury the reality,
Making myself the mystery,
A strong facade disguising the misery.
Empty, but beyond the point of emptiness,
Full to brim with fake confidence,
A guard that will never be broken,
Because I broke a long time ago.
I’m hurting but don’t tell anyone.
No one needs to know.
Don’t show or you’ve failed.
Always okay, always fine, always on show.
The show must go on.
It will never stop.
The show must not go on,
But I know it will.
I give up. I give up giving up.
I am lost.
I don’t need to be saved,
I need to be found.
POEM TITLE: WHO AM I TRYING TO BE?
ARTIST NAME: Cara Delevingne
ARTIST INFO: Cara Delevingne, actress and model, shares her personal experiences with anxiety and depression.